- Intrauterine devices are small T-shaped contraceptive devices meant to be placed in your uterus.
- IUDs have a 99% efficacy rate and are safe to use; however, they might disrupt your vaginal microbiome.
- IUDs may increase the chances of vaginal infections such as BV and vaginal yeast infections.
- BV can be prevented by practicing good hygiene, using probiotics, avoiding multiple sex partners, and discontinuing chemical and fragranced products.
Intrauterine contraceptive devices (IUDs) are becoming more popular among women searching for simple contraceptive options. Healthcare providers tout how easy they are to use, that they’re 99 percent effective at preventing pregnancy, and their relative lack of side effects as reasons why IUDs are a great option for most women. But while many people who have an IUD do not have any negative side effects, some women experience significant side effects including irregular bleeding patterns, unusual vaginal odor (especially with copper IUDs), and, in some cases, vaginal infections.
What’s the link between IUDs and vaginal infections, and how can you know if it’s safe to get one? In this article, we’ll discuss this common form of birth control and its correlation with different types of vaginitis so you can make the best decision for your overall wellness.
What Are IUDs?
IUDs are small t-shaped contraceptive devices made of copper. They’re a type of birth control that’s placed directly within the uterus. IUDs, along with the implant method, are the most effective contraceptive method. (1) They’re significantly more effective than vaginal sponges and condoms as well as other hormonal contraceptives like vaginal rings and birth control pills, meaning you are least likely to get pregnant while using an IUD. Only one out of 100 women having sexual activity get pregnant within their first year using an IUD.
To use an IUD, a healthcare provider must place the device in your uterus at a medical appointment. Placing a copper device might sound very invasive and painful, but most people don’t experience any complications after insertion, including pain.
Different Types of IUDs
In the United States, there are four IUDs approved for contraceptive purposes: one non-hormonal copper-bearing IUD and three levonorgestrel-releasing IUDs (a hormonal birth control).
- Copper-bearing IUDs are made of copper and plastic. These are non-hormonal, so they won’t impact your body’s natural hormone balance. The copper in the IUD acts as a spermicide to kill sperms before they reach the uterus, preventing pregnancy.
- Progestin levonorgestrel-releasing IUDs release hormones that cause the uterus lining to become thin and cervical mucus to become thick. Thick mucus prevents the sperm from reaching the egg or fertilizing it.
IUDs are one of the most common forms of birth control after sterilization (such as a hysterectomy or vasectomy); about 10.4 percent of women in the United States use IUDs for contraception. (2) Worldwide, over 159 million women use an IUD to prevent pregnancy. (3)
The Benefits and Drawbacks of Using an IUD for Birth Control
It can be hard to choose the best birth control method for you. Weighing the benefits against the potential drawbacks can help you make the most informed decision.
The benefits of using an IUD include:
- Effectiveness. IUDs are the most effective reversible contraceptive method for preventing pregnancy. Unlike sterilization, the effects of an IUD can be reversed if you decide you want to get pregnant in the future. To reverse the effects, your healthcare provider will simply remove it in their office.
- Hormone free. Some people don’t like the effects hormonal birth control methods may have on their physical or mental wellbeing. Copper-bearing non-hormonal IUDs can instantly provide contraception without impacting your hormone balance.
- Easy to use. Unlike the birth control pills, you don’t have to remember to use contraception every day to prevent pregnancy. Once an IUD is placed in your uterus, it can provide consistent birth control for anywhere from 3–10 years, depending on the type of IUD placed.
Not everyone experiences all of the below IUD drawbacks, but you won’t know until you get one placed. Here are the top complaints about IUDs:
- Side effects. Some women might experience mild cramps, abdominal pain or pelvic pain, and vaginal bleeding in the first few weeks after the IUD is placed.
- Impact to menstrual period. Some women get shorter periods, some experience absent periods, and some experience heavier periods, particularly individuals using the copper IUD.
- Limitations. Unlike condoms, IUDs do not provide protection against sexually transmitted infections (STIs), so additional protection methods are necessary when engaging in sexual intercourse.
- Increased infection risk. IUDs can disrupt your vaginal microbiome, which may increase your risk of yeast infections and bacterial infections such as bacterial vaginosis (BV).
- Increased vaginal pH. Irregular bleeding may cause your vaginal pH to increase, making you more vulnerable to vaginal infections like BV or STIs.
IUDs and Vaginal Infection Risk
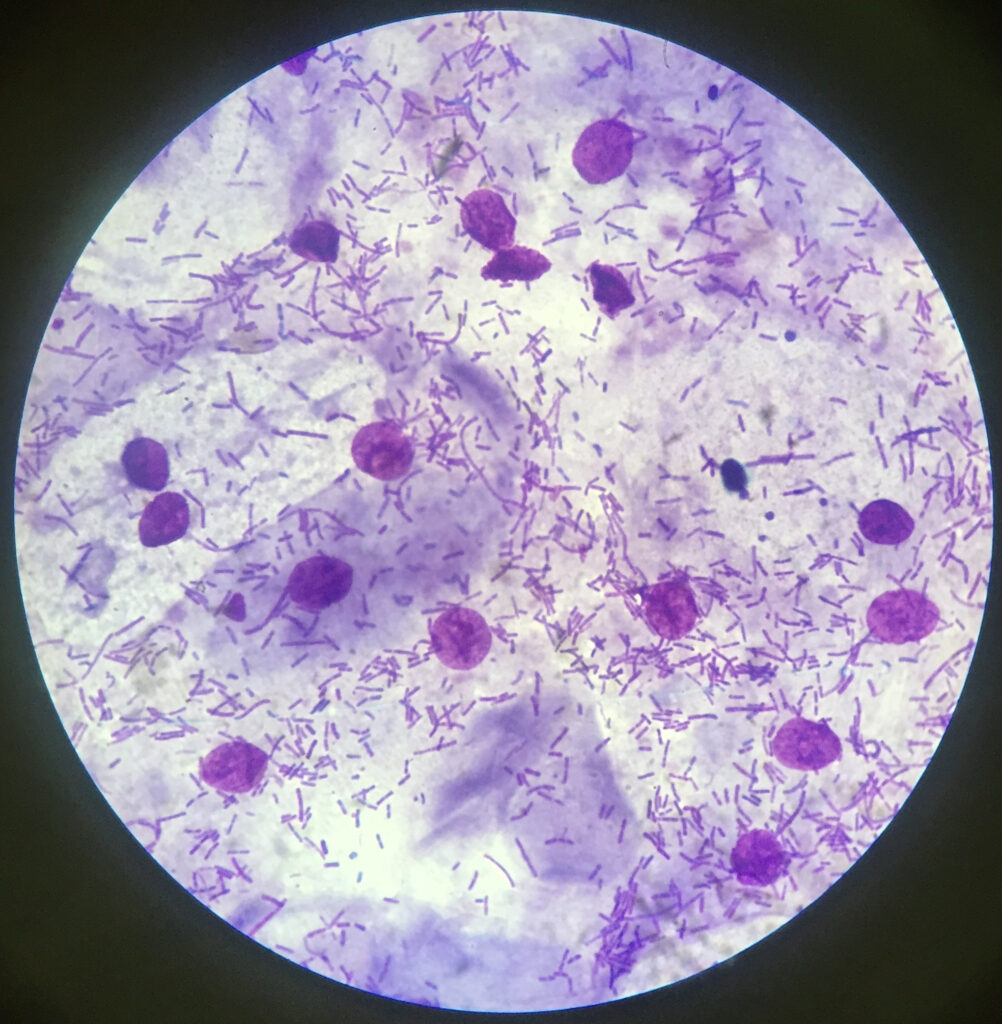
In order to understand how IUDs can increase your risk of common vaginal infections, you need to understand the interaction between infections and your vaginal microbiome. The vaginal microbiome is your vagina’s unique mix of microorganisms that populate it.
At all times, your vagina is populated by trillions of aerobic and anaerobic bacteria. Good bacteria coexist with potential harmful anaerobic bacteria in your vaginal tissues. In the vagina, the most common type of good bacteria present is called lactobacillus.
When lactobacillus levels are high, they keep the growth of bad infection-causing bacteria in check, reducing your risk of infections. However, this stable vaginal microbiome can be easily disrupted due to:
- Hormonal changes you experience as a result of contraceptive methods or during menstruation
- Use of vaginal care products such as douches, vaginal washes, and scented vaginal soaps
- Unprotected sexual interactions with new or multiple sexual partners
- A poor diet rich in sugar and fats
- Use of medications such as antibiotics
However, it’s not all bad news: your body is prepared to rebalance its vaginal microbiome in response to bacterial imbalances. For instance, the vagina produces vaginal discharge, which rinses it of bad bacteria.
Vaginal pH and Infections
The dominant good bacteria lactobacillus naturally produces lactic acid and hydrogen peroxide. These acids keep the vaginal environment acidic, which also helps prevent the growth of bad bacteria. However, many things can increase the vagina’s pH and make it more likely that bad bacteria can grow and thrive, including:
- Unprotected sex. Semen has a higher pH than the vagina, so the presence of semen in the vagina may increase its pH.
- Your menstrual period. Period blood also has a higher pH than the vagina. Increased bleeding, which may occur with an IUD, can increase the vagina’s pH, as can leaving in tampons or menstrual cups for long periods.
- Douching. Because douching wipes out all bacteria from your vagina, including good lactobacillus strains, it can inadvertently raise your vaginal pH and increase your risk of infection.
- Antibiotics. Like douching, antibiotics don’t selectively target bad bacteria—they kill good bacteria too. A lack of lactobacillus in the vagina increases the vaginal pH.
What Do IUDs Have To Do With the Vaginal Microbiome?
To sum it up, IUDs can negatively impact your vaginal health in one of three ways:
- Irregular vaginal bleeding patterns can increase the amount of menstrual blood present in your vagina, which can raise your vaginal pH and increase your risk of infection. (4)
- The hormonal changes resulting from IUDs can slow the growth of good bacteria, increasing your susceptibility to infection. (5)
- Insertion of an IUD may increase the number of harmful bacteria in your vagina, increasing your risk of infection.
IUDs and BV
Statistically speaking, an increased chance of developing a vaginal infection puts you most at risk of developing bacterial vaginosis, since it’s the most common vaginal infection. (6) While vaginal yeast infections, urinary tract infections, and even STIs may be more likely using an IUD, BV is most likely. So what is BV, and how can you tell if you have it?
BV is an infection caused by an imbalance between good and bad bacteria residing in your vagina. Sound familiar? Health experts call BV a form of vaginal dysbiosis, which means an imbalance of normal microbiomes. BV is a highly treatable condition, but if untreated it can lead to significant problems including pregnancy complications and an increased risk of developing an STI. (7)
A few significant studies have examined how IUDs may cause BV:
- One study compared the prevalence of BV in women having IUDs with those who take oral contraceptives. (8) The results showed a three-fold increased chance of BV in women using IUDs.
- An article published in Evidence-Based Practice concluded that between 7–47 percent of women using IUDs have BV, while only 2–35 percent of women using oral contraceptives do. (9)
Symptoms of BV
According to data collected by the Centers for Disease Control and Prevention, about 84% of women living with BV do not exhibit any symptoms. (10) Symptomatic women may experience:
- Vaginal discharge with an unusual odor often described as a fishy smell
- Itching around the vaginal opening or vulva
- A burning sensation while peeing
- Thin vaginal discharge that’s a grayish color
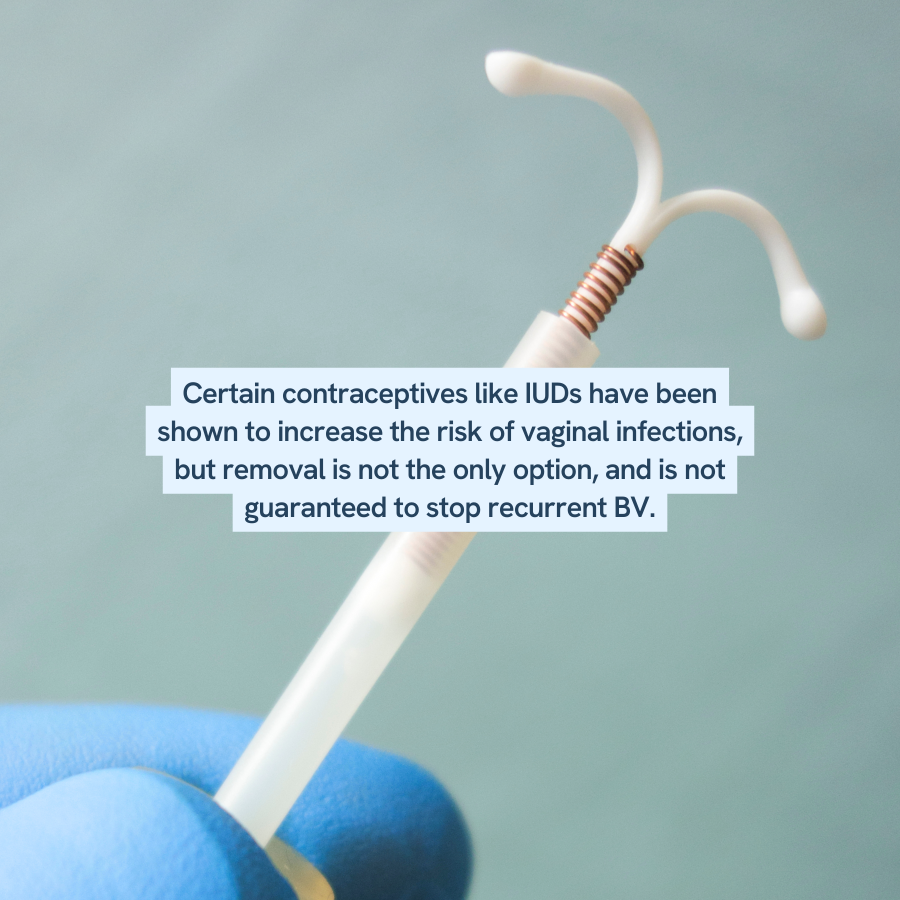
Preventing BV From an IUD
If you believe an IUD may be causing you to have a BV infection, it’s important to share your concerns with a healthcare provider. If you decide to keep your IUD, stick to these BV prevention methods to minimize the likelihood of recurrent BV infections:
- Practice good vaginal hygiene, including wiping from front to back and washing your vagina regularly with warm water
- Avoid the use of harsh chemicals found in soaps, shampoos, or vaginal washes on your vagina
- Eat a healthy diet rich in probiotics, fiber, vegetables, and fruits
- Always use protection when having sex, and avoid having multiple sex partners, since this increases your exposure to potentially harmful bacteria
- Quit douching to preserve your lactobacillus levels

Our Happy V® Prebiotic + Probiotic was created for anyone who is experiencing symptoms related to Bacterial Vaginosis and Yeast Infections. Eliminate the odor, itch, gut bloating, and other symptoms.
Happy V Probiotic
This is your foundation! Happy V Probiotics are packed with six specific strains that introduce good bacteria to optimize the pH level of your vaginal flora.
Safeguard Your Vaginal Health With Support From Happy V
A lot of factors can impact your vaginal health, but there’s one clear way to protect it—take probiotics for vaginal health. Prebiotics and probiotics help your body restore and grow healthy bacterial levels, which ultimately protects you from infection. When paired with healthy lifestyle practices like safe sex, a nutritious diet, and good vaginal hygiene, probiotics for women can help restore your happy v.
- https://www.acog.org/womens-health/infographics/effectiveness-of-birth-control-methods
- https://www.cdc.gov/nchs/fastats/contraceptive.htm
- https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_contraceptiveusebymethod_databooklet.pdf
- https://pubmed.ncbi.nlm.nih.gov/17152227/
- https://www.tandfonline.com/doi/abs/10.1080/17512433.2021.1917373
- https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm
- https://americanpregnancy.org/healthy-pregnancy/pregnancy-complications/bacterial-vaginosis-during-pregnancy/
- https://pubmed.ncbi.nlm.nih.gov/11704096/
- https://journals.lww.com/ebp/Abstract/2018/07000/Is_the_risk_of_bacterial_vaginosis__BV__increased.17.aspx
- https://www.cdc.gov/std/bv/stats.htm#:~:text=Most%20women%20found%20to%20have,lifetime%20number%20of%20sexual%20partners.
- A-
- A+