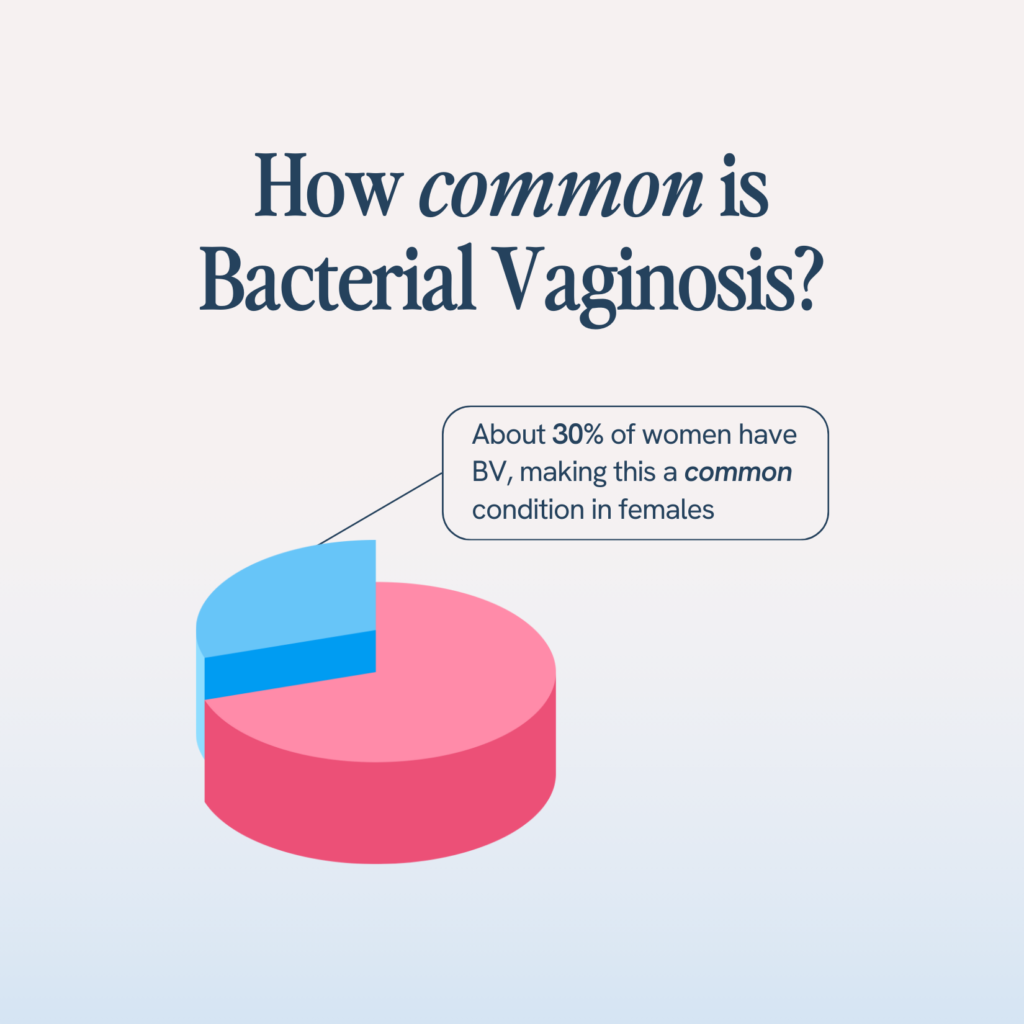
- Bacterial Vaginosis is the most common vaginal infection that affects nearly 21M women every year in the United States. It’s nothing to worry about.
- There are two theories as to how Bacterial Vaginosis occurs. The first is that the pH of the vaginal flora changes causing colonies of hydrogen peroxide-producing Lactobacillus (good bacteria) begin to die within the vaginal flora and harmful bacteria (anaerobes) begin to thrive. The second is that because Lactobacillus die off for other reasons, pH changes, allowing anaerobic bacteria to colonize the vagina.
- Common symptoms of Bacterial Vaginosis(BV) includes discharge, an unusual or foul odor, itch and a change in vaginal pH.
- Because lactobacillus colonize begin to decrease, there is less lactic acid and hydrogen peroxide being produces, which means Bacterial Vaginosis can lead to an increase in catching sexually transmitted diseases (STD’s).
- Natural remedies, such as Probiotics, Prebiotics and Cranberries aim to treat the symptoms of BV, UTIs, and yeast infections while minimizing re-occurrences.
Over 21 million women in the US struggle with BV ever year but because no one is talking about it, BV continues to feel like a mystery. If you are currently struggling with BV, you are far from alone.
So… let’s talk about it! This article right here is your ultimate guide. We’re breaking the silence on BV and diving deep so you can understand what’s going on and how to navigate it better. This guide doesn’t replace a doctor, but it’s a great starting point to break the stigma and begin advocating for your health and also stop possible bad habits- I say this because I find my patients do not even realize the things they do that contribute to BV.
What is BV?
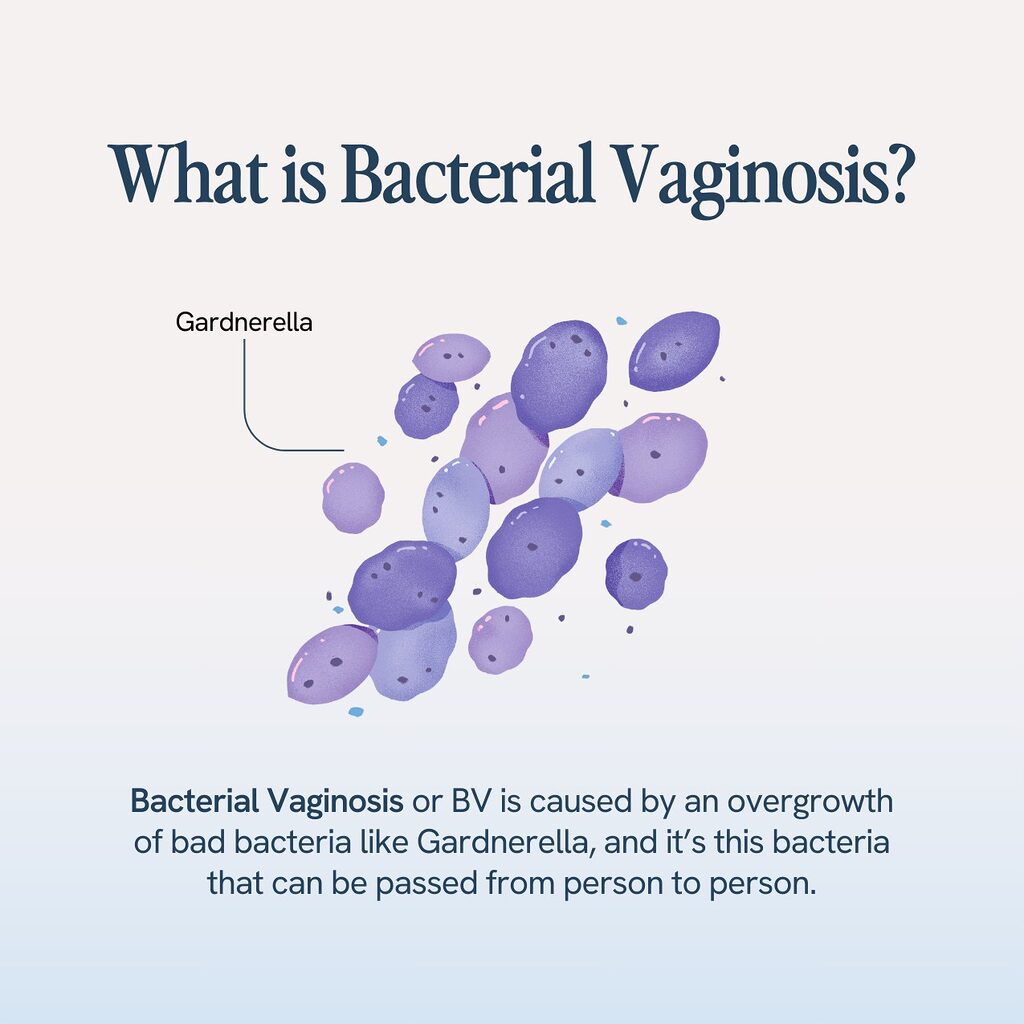
Let’s start with the basics here and talk about what BV actually is. In the simplest of terms, bacterial vaginosis is a bacterial infection that affects the vagina. And we want to be super clear that even though BV affects a sexual organ, it is NOT a sexually transmitted disease or STD, so rest easy there.
BV happens when there’s a shift or imbalance in the vaginal microbiome, meaning the bacteria in your vagina. One of the reasons that it’s so common is that the vaginal microbiome is delicate, and many things can disrupt the natural balance of helpful bacteria 1 in your vagina. (As for what those things are, we’ll get into those a bit later.)
As the Journal Reviews of Obstetrics and Gynaecology2 notes, BV occurs from dysbiosis, or the “loss of the normal bacterial population of the vagina and their replacement by other species”. And when bad bacteria outweigh the good, it leads to an infection, or BV.
What is the Vaginal Flora?
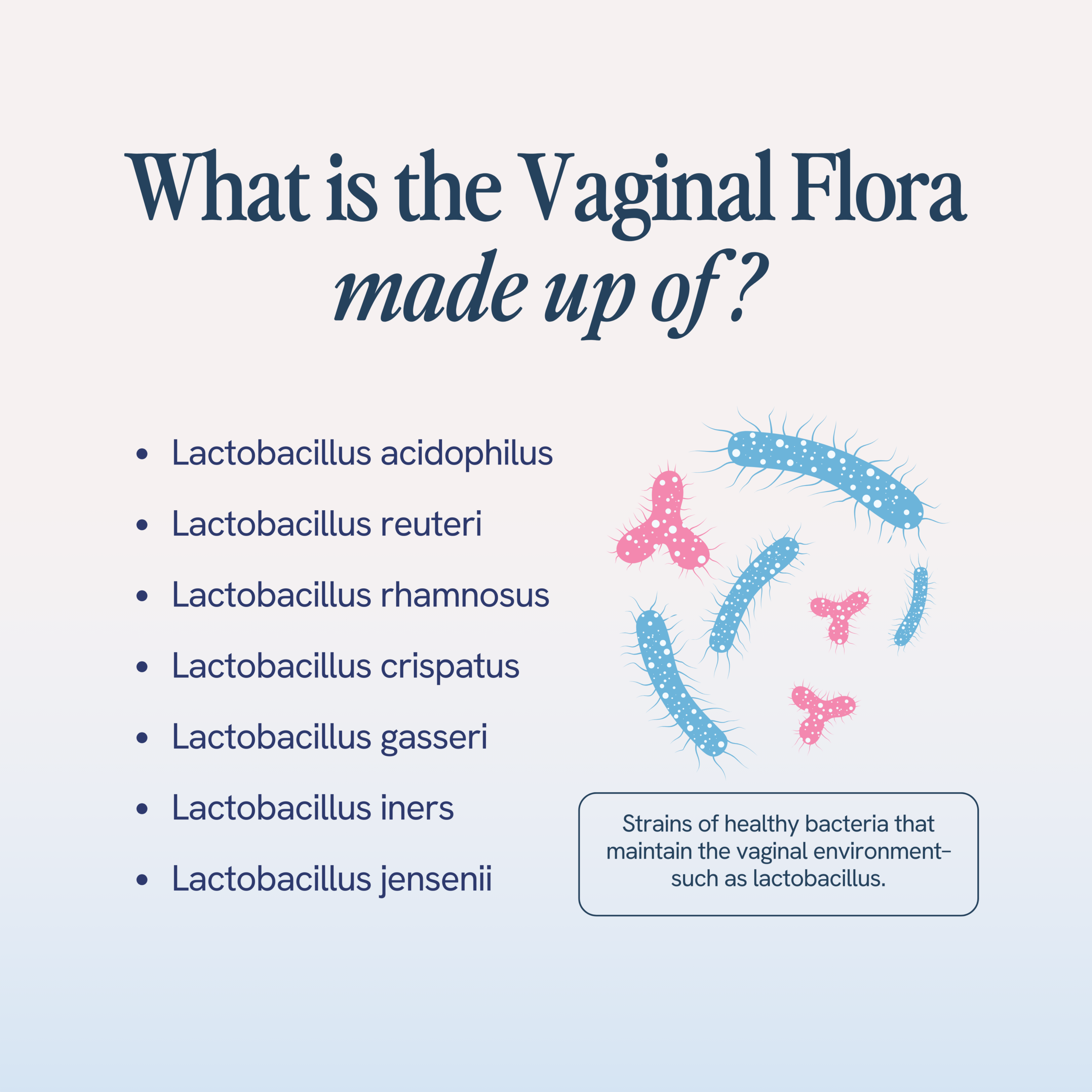
Your vaginal flora is another word to describe your vaginal microbiome, which you will remember is the makeup of bacteria that occupy the vagina. Think of it kind of like your vagina’s ecosystem. When this ecosystem is healthy, the helpful bacteria have the climate and environment they need to live, thrive, and reproduce.
The helpful bacteria that we are most concerned about in this ecosystem are probiotics. Probiotics are responsible for all kinds of things in your body. Probiotics are often referred to in terms of gut health and digestion, but these same probiotics, like Lactobacilli, are also responsible for maintaining vaginal health. For lactobacilli to thrive, they need a vaginal pH level of around 4.5.
What is Vaginal pH?
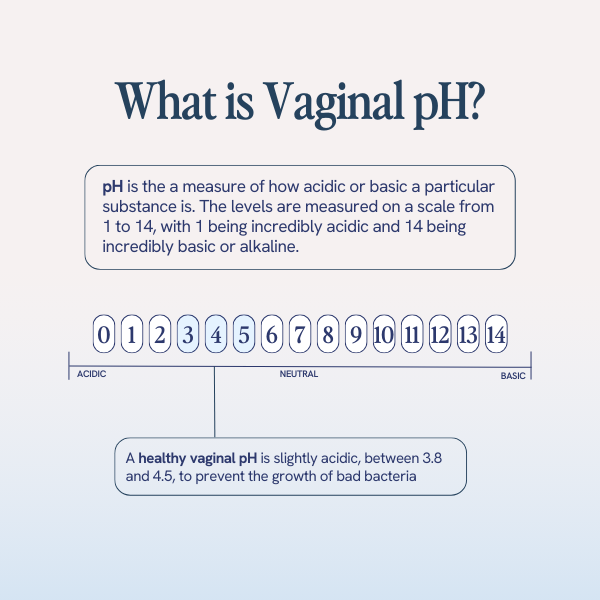
If your vaginal flora is your vagina’s ecosystem, the vaginal pH is the climate of that ecosystem. But instead of being hot & cold, the climate within the vagina will either be acidic or basic, depending on where it falls on what’s called the pH scale.
The pH scale goes from 1-14, 1 being the most acidic (think: battery acid and lemons) and 14 being the most basic or alkaline (think: soap and bleach). A pH of 7 is a neutral pH, often the pH of water. The ideal vaginal pH is between 3.8 and 4.5. This is slightly acidic, which may have you thinking, “I don’t want acid in my vagina!” but this slight acidity is a good thing. It is a sign you have enough of that healthy probiotic Lactobacillus to keep things working optimally.
What’s the link between probiotics and Vaginal pH?
As we said earlier, Lactobacilli probiotics are vital for maintaining vaginal health and the balance of bacteria. That’s because Lactobacilli actually convert prebiotic glucose, their food source, in the vagina into lactic acid, hydrogen peroxide, and bacteriocides. These natural defenses they produce help maintain that slightly acidic pH, which naturally prevents the overgrowth of bad bacteria.
What happens in your vaginal flora when you get BV?
If you’ll remember, BV is essentially a disruption to your vaginal flora, but let’s break down exactly what that disruption looks like.
Essentially, when you get BV, something happened that caused your vaginal pH to become less acidic than it should be. It’s shifted the climate in your vaginal ecosystem, and this new climate allowed harmful bacteria, known as anaerobes, to overtake that ecosystem of your vaginal flora.
As for what caused that initial shift in vaginal pH, there are a whole host of potential causes (see below), but the path to BV is the same: a change to pH = a new vaginal climate, and a new vaginal climate = the overgrowth of bad bacteria.
What causes BV?
There’s no shortage of potential causes for BV, which is why it is so incredibly common. Some causes are related to lifestyle and can be changed; some are simply part of female biology. The following are common risk factors related to bacterial vaginosis:
- Eating Habits: This is by far the #1 cause of BV. When you don’t eat enough nutritious foods, the lactobacilli don’t get the nutrients they need to do their job and maintain a healthy vaginal pH. So, if you have been struggling with BV, take a look at your diet. Changing your eating habits isn’t always easy, but it can make a world of difference to your vaginal health. Prioritize low-glycemic carbohydrates, probiotic-rich foods like yogurt, prebiotic-rich fibrous foods, and antioxidant-filled fruits.
- Clothing Choices: Does this sound like you: you end a HIIT workout or spin class, then immediately jump in the car to run some errands? We’re all guilty of doing this at some point, but staying in damp, moist clothes (especially underwear) can be the perfect breeding ground for anaerobic bacteria – making it one of the easiest ways of getting BV. So try to make time for a shower and a change of clothes any time you exercise, spend time at the pool or beach, or work up a sweat outside. Also, if you are wearing panties made of a synthetic material like nylon, consider making a switch to cotton, which is much more breathable and will prevent some of that moisture retention.
- Personal Care Products: Certain personal care products, like vaginal deodorants, can have chemicals that can change the pH of the vaginal flora, putting you at higher risk for infections. We recommend opting out of any kind of vaginal rub or deodorant — especially any scented kinds — and just use a mild soap to clean the vulva area when necessary.
- Sex Partner and Number of Sex Partners: While the vagina is slightly acidic, semen is basic, and the role of semen is actually to temporarily change your vaginal pH to allow sperm to swim easier. But frequent unprotected sex or sex with multiple partners and multiple microbiome identities can make this temporary change to your pH not-so-temporary. We aren’t saying you need to change everything about your sex life — love is love, and you should do what makes you happy. What we are saying, though, is that if you are struggling with BV, you should start a conversation with your sexual partner or partners about how you can get healthy together.
- Sex Toys: Now, sex toys themselves aren’t the problem, so if they provide you with a sense of fun or adventure, keep right on using them. Just make sure you clean them properly after every use since improperly cleaned sex toys can introduce harmful types of bacteria into your vaginal microbiome.
- Your Menstrual Cycle: As if your period isn’t annoying enough, right? Your menstrual cycle can disrupt your pH because menstrual blood is incredibly basic, with a pH over 9. While you can’t exactly just not have your period anymore, you can mitigate the risk of BV by changing your tampons or pads frequently. Think: every 2-4 hours.
- Antibiotics: Antibiotics work by not just killing the bad bacteria causing an infection but by killing all the bacteria in your body, including that healthy Lactobacillus we discussed earlier. And without Lactobacillus to maintain a healthy pH, you are more prone to getting BV and yeast infections. If you are ever prescribed an antibiotic, we recommend offsetting it with a good probiotic supplement, especially one with Lactobacillus, to reintroduce that into your vaginal microbiome.
- Estrogen Levels: If none of the above feel like they are the potential cause of your BV, it may be time to visit a doctor and check your hormone levels since low estrogen can cause changes in your microbiome. Your doctor can advise you on any potential hormone replacement therapy.
What bacteria causes BV?
We mentioned the word anaerobes when talking about harmful, BV-causing bacteria earlier, and there are many, many types of anaerobic bacteria out there. The most common vaginal bacteria when it comes to BV is called Gardnerella vaginalis.
The way Gardnerella vaginalis works is by adhering to the vaginal mucosa in your vaginal wall. From there, they can multiply and over-consume glucose, inhibiting lactobacilli from making their natural defenses (lactic acid, hydrogen peroxide). What’s also kind of interesting/terrifying about G. vaginalis, in particular, is that it may also create symbiotic relationships with formerly dormant vaginal anaerobes, causing further complications.
One study found that G. vaginalis may activate dormant E.coli bacteria, leading to an increased risk of UTIs6 (check out our blog post on “The Difference Between UTIs & BV: Causes and Prevention Tips”).
While Gardnerella is the most common culprit for BV, other bacteria, such as Prevotella, Peptostreptococcus, and Mycoplasma, can all cause BV.
Who gets Bacterial Vaginosis?
To make a long story short, anyone with a vagina can get BV. But it is far more common in people who are sexually active, in part because of the ways that sex can alter the microbiome, like we noted earlier, and also in part because there is evidence that shows that the common BV-causing bacteria Gardnerella can be transmitted sexually.
With the Centers for Disease Control and Prevention (CDC) clocking incidence at over 21 million people a year, BV is the most common vaginal infection. But of the 21 million people who experience it, only 50% will notice any symptoms. That’s why it’s essential to have regular visits with your gynecologist or primary physician. They will screen for asymptomatic BV and help prevent it from becoming a larger issue. As for what those larger issues could be, we’ll get into those in a bit.
Is BV an STD?
No. Though there is a strong link between sex and BV, both due to the high pH in semen and the potential transfer of G. vaginalis, BV is NOT an STD.
However, it is important to note that having sex with an active BV infection can increase your chances of getting a sexually transmitted infection (STI) or sexually transmitted disease (STD) like herpes, chlamydia, or gonorrhea7. That’s because the presence of BV indicates that your natural defenses are compromised. You have an unhealthy vaginal flora, with insufficient lactic acid or hydrogen peroxide present to fight off infection.
What are the signs and symptoms of Bacterial Vaginosis?
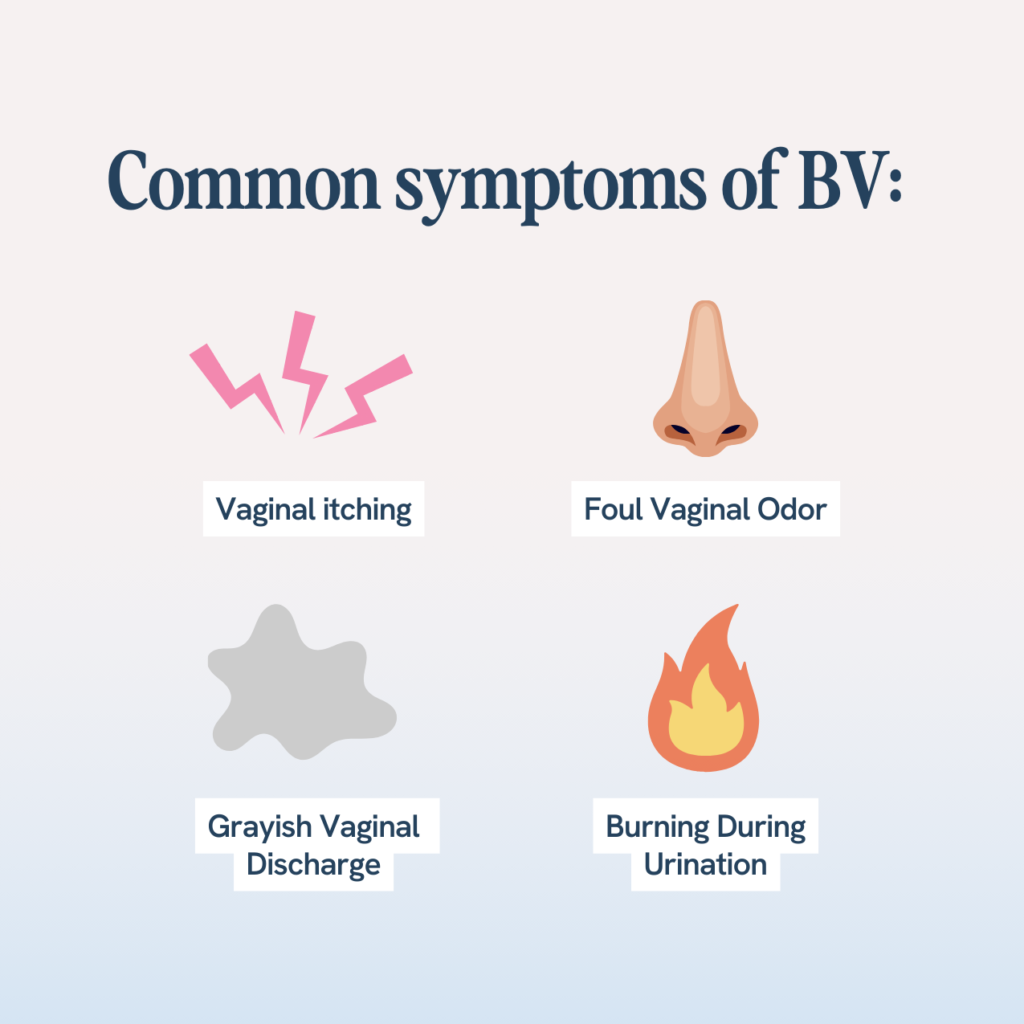
So remember, half of all people with an active BV infection show no symptoms at all, which is why it’s so important to maintain regular visits with your gynecologist.
As for the other half of people who do experience symptoms, the symptoms tend to vary from person to person. Some people only experience one of these symptoms, while others experience multiple. The most common symptoms of BV include:
- An unusual or unfamiliar odor that some refer to as a fishy smell
- Vaginal discharge (also known as vaginal fluid) that’s generally thin and grayish and increases with sexual activity
- Burning and itching while urinating
Now, if you’re thinking, “Wait, those also sound like symptoms of a yeast infection or UTI,” that’s because they are. BV shares symptoms with vaginal yeast infections, urinary tract infections, and Trichomoniasis, but all require different treatments in order to resolve them.
That’s why it’s so important to visit a gynecologist or primary care physician if you are experiencing any of these symptoms, so they can run some tests and get you a definite diagnosis.
When should you see a doctor for BV?
As we said, if you are experiencing any of the symptoms we listed above, make an appointment with your doctor or healthcare provider. So make an appointment if:
- You notice unusual vaginal discharge or vaginal discharge that’s associated with an odor, discharge, color, vaginal itching, or burning sensation.
- You’ve had vaginal infections before, but this occurrence comes with new symptoms, such as odor, abnormal vaginal discharge, vaginal itching, or burning sensation.
- You have a new sex partner, multiple sex partners, or past partners who have had bacterial infections.
- Over-the-counter or home remedies are not treating the symptoms.
What happens if BV is left untreated?

I would suggest mentioning PID, Increased risk of infection after procedures and increased susceptibility to STI’s first, then possible OB complications last.
The good news is that bacterial vaginosis is a treatable infection when appropriately diagnosed. But if left untreated, it can cause much larger health issues. That’s because when the bacteria causing BV grow and multiply on the vaginal wall, they can actually hide and nurture other harmful bacteria that may be living underneath.
And because these other harmful bacteria are, in essence, hidden by the BV-causing bacteria, they are less exposed to antibiotics, antimicrobials, and other natural remedies you may be using to treat them.
More specifically, untreated bacterial vaginosis has been linked to a greater risk of:
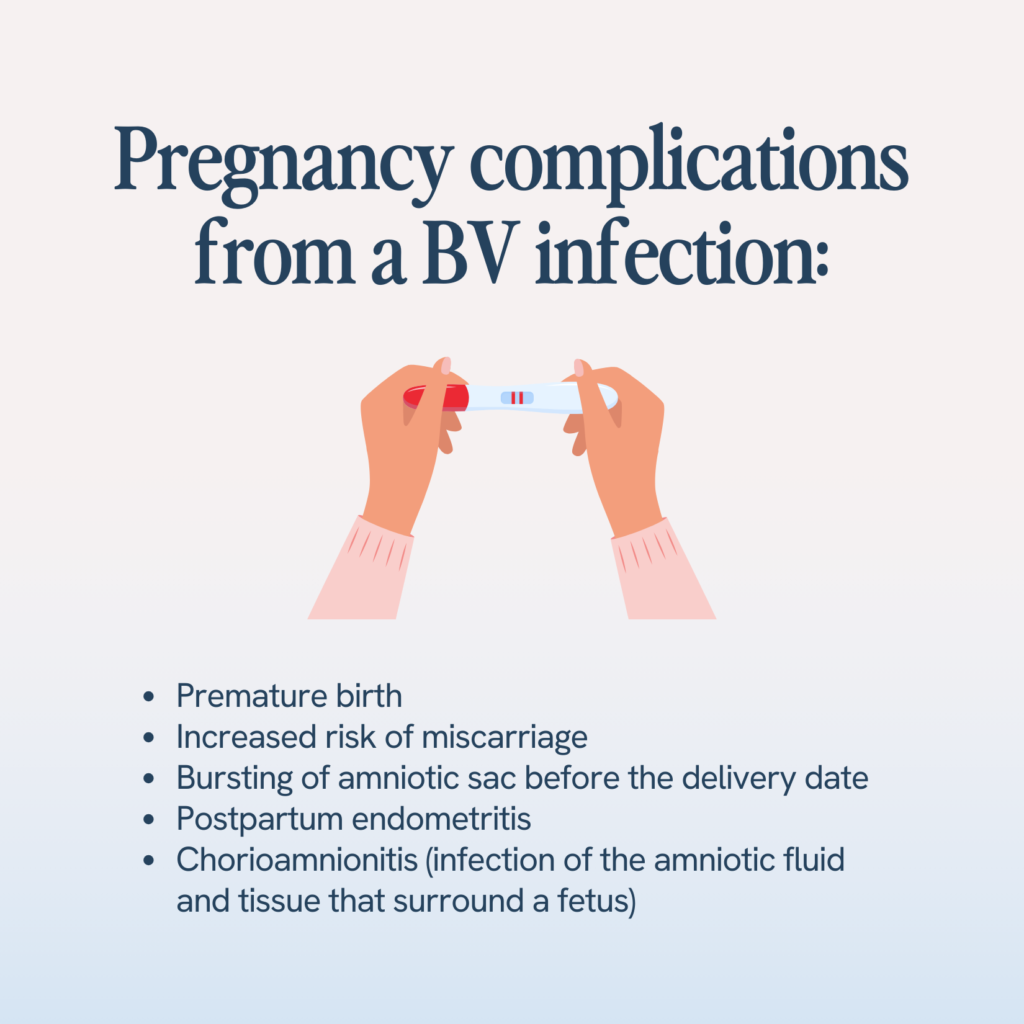
- Pregnancy complications: One 2006 study⁸ on BV and pregnancy found that BV was associated with low birth weight and small size.
- Sexually transmitted infections: We mentioned this before, but it’s worth reiterating. According to the Centers for Disease Control, having BV can increase your chances of acquiring an STD. This includes herpes, chlamydia, gonorrhea, and even HIV. It also increases your odds of passing these viruses to a partner.
- Infection risk after gynecologic surgery: According to the Mayo Clinic, having Bacterial Vaginosis may increase the risk of developing an infection following procedures like hysterectomies or dilation and curettages (D&Cs).
- Pelvic Inflammatory Disease (PID): When left untreated, BV can lead to pelvic inflammatory disease or PID. PID is an infection of the female organs, such as the uterus and the fallopian tubes. PID also puts you at increased risk of infertility.
- Development of biofilm & BV recurrence: The bacteria that causes BV, like Gardnerella vaginalis, can form what’s called a biofilm. This biofilm will actually protect the G. vaginalis from antibiotics and other forms of treatment, making it more challenging to treat. It can also contribute to the high rates of recurrence seen with BV, as residual bacteria within the biofilm can multiply and cause a new infection after the end of treatment.
How is Bacterial Vaginosis diagnosed?
A doctor or gynecologist best diagnoses BV, so make an appointment if you experience any of the symptoms we mentioned earlier.
In your appointment, your doctor may:
- Perform a physical examination
- Ask about your hygiene routine
- Evaluate your medical history and sexual activity
- Perform a pelvic exam if needed
- Get swab test samples to rule out other sexually transmitted infections such as gonorrhea or trichomoniasis.
In these tests, they will look for four clinical criteria9 that signal BV. These include:
- Vaginal discharge that’s homogeneous, meaning that it is the same throughout.
- The vaginal discharge has a pH greater than or equal to 4.5.
- The vaginal discharge has an ammonia-like odor when mixed with 10% potassium hydroxide.
- Vaginal discharge contains clue cells representing over or equal to 20% of vaginal epithelial cells.
How does a doctor treat Bacterial Vaginosis?
Once your doctor has confirmed a BV diagnosis, they will likely prescribe antibiotics to fight off the bacteria causing the infection.
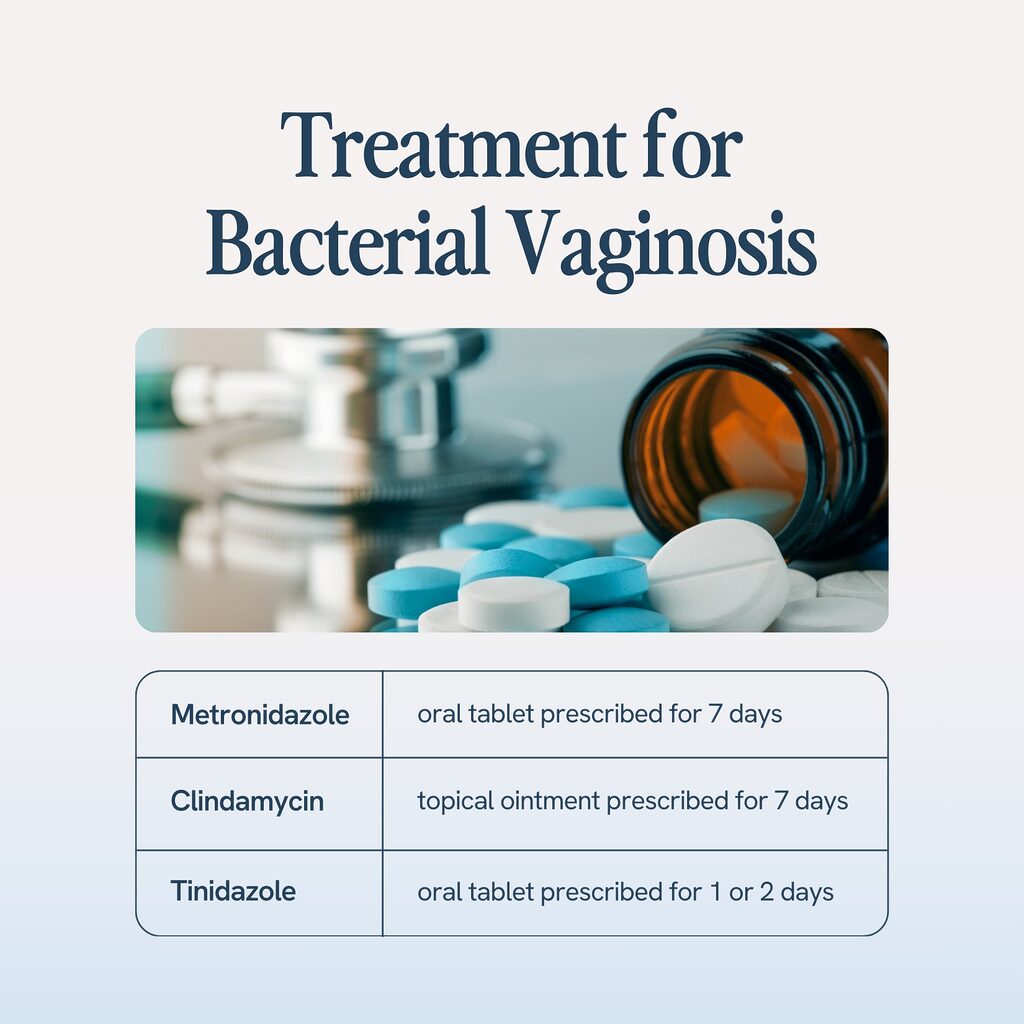
Common antibiotics for BV include:
- Metronidazole. This is the most commonly prescribed antibiotic and comes as a vaginal cream, gel, and pill.
- Tinidazole, which is similar to metronidazole.
- Clindamycin, which generally comes as a vaginal suppository or gel.
However, even after antibiotic treatment, nearly 60% of women diagnosed with Bacterial Vaginosis will experience it again. This is due to a few things. The first is the biofilm we talked about earlier, which can make it harder for antibiotics to effectively reach the harmful bacteria. But also, many of the root causes of BV are lifestyle-based, so without lifestyle changes, BV is likely to occur again. So, let’s talk about some important lifestyle changes you can make to prevent BV from coming back.
Are there any natural treatments for BV?
So, first, we want to reiterate that if you are struggling with BV symptoms and/or your doctor has prescribed antibiotics, those are going to be your best bet for getting rid of an active infection. But to minimize future occurrences and break the cycle of BV, look to some of these proven natural remedies.
Vaginal probiotics
Probiotics, especially those that contain Lactobacilli, are essential for optimal vaginal health, especially if you struggle with BV. You can get these probiotics through foods like yogurt, kefir, and fermented foods like kimchi, but many find it easier and more effective to take a daily probiotic supplement.
It can also help to take a probiotic that also includes prebiotics. Prebiotics are the dietary fibers and glucose that probiotics consume to make lactic acid and hydrogen peroxide. Essentially, the prebiotics feed the probiotics and make sure they are functioning properly.
If you are looking for a probiotic that contains both Lactobacillus and prebiotics, Happy V has you covered. Our Prebiotic + Probiotic was formulated to include the 7 most clinically studied probiotic strains to get your pH levels back to normal quickly.
Check out Happy V Pre+Pro for a product made with clinically proven vaginal probiotic strains proven to alleviate the symptoms of BV
Cranberry
You may have heard about cranberry products helping with UTIs, but they may help prevent BV recurrence as well. That’s because cranberries contain excellent antioxidants known as proanthocyanidins or PACs. These PACs prevent bacteria from creating that biofilm.
But our advice when it comes to cranberry? Skip the sugary cranberry juice. Instead, opt for a supplement like Happy V’s D-Mannose+Cranberry capsules or D-Mannose+Cranberry Stick Packs. These can be taken daily and will help you begin flushing bad bacteria from your body.
Lifestyle Changes: How to Prevent Bacterial Vaginosis
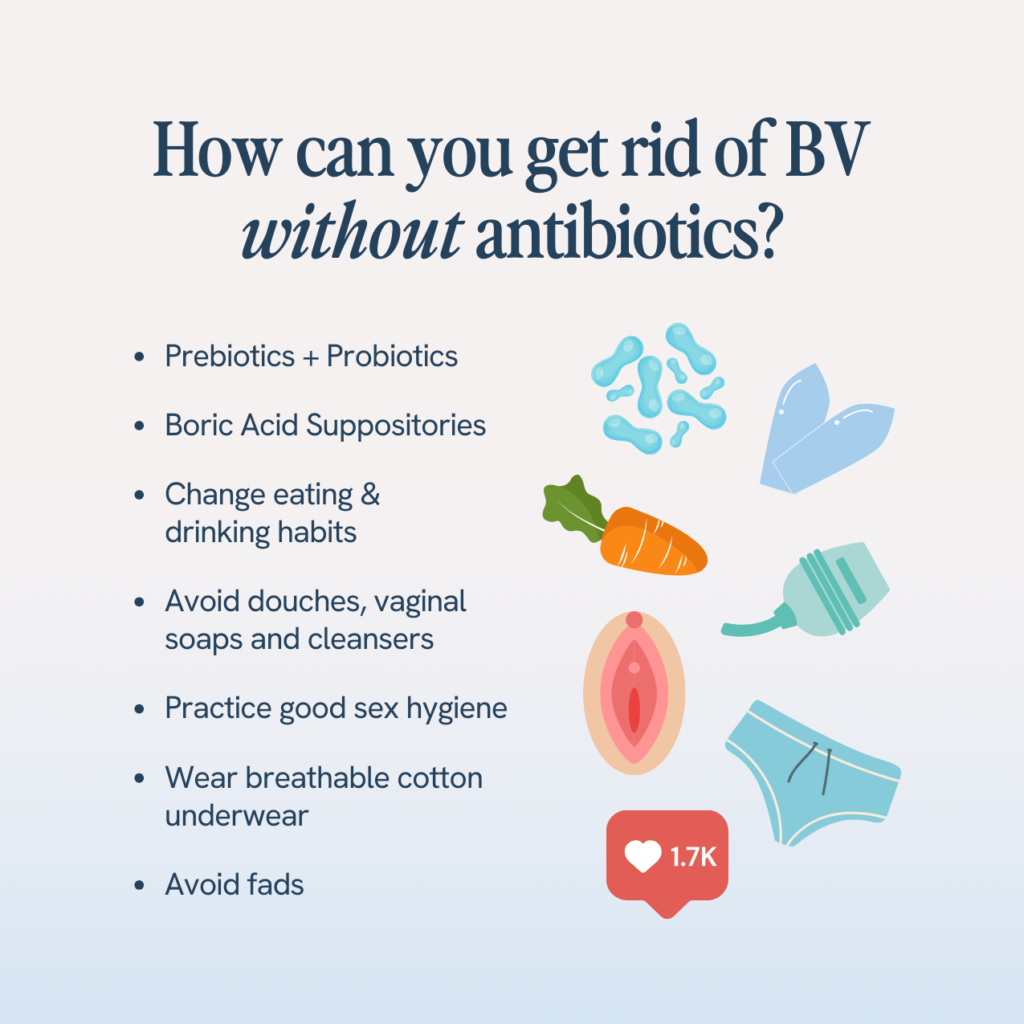
Along with these natural remedies, there are other lifestyle changes to consider that can prevent future BV occurrences and minimize the risk of other health problems as well. These include:
- Changing up your birth control method. Make no mistake, we support safe sex! But certain chemicals in condoms, vaginal lubricants, and spermicides can disrupt your vaginal pH and encourage bad bacteria to grow. And if you use an IUD, studies12 have shown these can increase your chances of getting BV. So, if you are struggling with BV and can’t seem to pinpoint the root cause, consider changing up your birth control method and seeing if that helps.
- Buying new underwear. Tight underwear, especially those made out of synthetic fibers, don’t allow your vagina to breathe, which can increase the risk of infection. Consider switching to a more breathable cotton.
- Stopping douching. Douching is the process of using water or other chemicals to clean your vagina, but the vagina actually self-cleaning. And introducing anything into the vagina can disrupt your vaginal pH. The healthiest way to clean and clear your vagina from unwanted infections is to simply wash your vulva with mild, unscented soap or just plain water.
- Avoid foods high in sugar. Bad bacteria love glucose, so either reduce the added sugars in your diet or remove it altogether. Remember, added sugar isn’t just in food but in drinks like alcohol.
- Changing your tampons, pads, or menstrual cups more frequently. Remember that the pH of menstrual blood is much, much higher than that of the vaginal flora, so letting the blood sit in the same area for too long can increase your normal pH.
- Changing out of clothes following a swim or exercise session. Bacteria love warm, moist, and humid environments. So don’t just sit around in wet clothes; change and keep your vaginal area as dry as possible.
- Switching to unscented products. Just as scented tampons or pads can irritate your skin, soap, laundry detergents, and scented or colored toilet paper can also make you more susceptible to vaginal infections.
- Changing the way you wipe. Properly wiping after each bathroom use can help decrease BV recurrence. In short, wipe your anus from front to back, and use different toilet paper between your vagina and anus.
- Practicing Safe Sex. Using Latex condoms, talking to your partner or partners, limiting your number of sex partners, and urinating after sex are all ways that you can help minimize the risk of potential BV and UTI episodes.
Medical factors
Excessive usage of certain medications and devices can also cause an imbalance in your vaginal flora.
- Antibiotics treat infections caused by harmful bacteria but can also kill off good bacteria. This makes you susceptible to other types of conditions.
- Studies show that having an IUD (contraceptive device) can increase your chances of getting Bacterial Vaginosis. If you have had an IUD, inform your doctor when seeking treatment.
Conclusion
So, by now, you have read so much about BV, you are probably feeling like a pro… and that’s the point! We hope this guide has taken the stigma out of this super common infection and given you the tools you need to seek treatment, advocate for your health, and prevent BV recurrence.
For more information about BV, you can visit the American College of Obstetricians and Gynecologists website. Remember, your doctor is going to be your best ally when it comes to an active BV infection, but our lines of communication are always open, too. If you have any questions, feel free to ask here.
Anaerobes — a microorganism that grows in low oxygen states.
Anaerobic Infection — common infections that are caused by anaerobes.
pH Scale — A scale that measures how acidic or basic a substance is that ranges from 0 to 14.
Alkalized — having the properties of being non-acid; having a pH above 7.
Acidic — having the properties of an acid; having a pH below 7.
Probiotics — living bacteria and yeasts that are beneficial for you, especially your digestive system and flora.
Lactobacillus — a rod-shaped bacterium which produces lactic acid and hydrogen peroxide from the fermentation of carbohydrates in order to multiply and stave off anaerobes.
Trichomoniasis — The most common and curable STD which affects the urinary tract, vagina, or digestive system.
Epithelium — A thin tissue that forms on the outer layer of a body’s surface and lining the alimentary canal and other hollow structures.
- Chen X, Lu Y, Chen T, Li R. The Female Vaginal Microbiome in Health and Bacterial Vaginosis. Front Cell Infect Microbiol. 2021;11:631972. doi:10.3389/fcimb.2021.631972
- Livengood CH. Bacterial vaginosis: an overview for 2009. Rev Obstet Gynecol. 2009;2(1):28-37.
- Borges S, Silva J, Teixeira P. The role of lactobacilli and probiotics in maintaining vaginal health. Arch Gynecol Obstet. 2014;289(3):479-489. doi:10.1007/s00404-013-3064-9
- Mijač VD, Đukić SV, Opavski NZ, Đukić MK, Ranin LT. Hydrogen peroxide producing lactobacilli in women with vaginal infections. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2006;129(1):69-76. doi:10.1016/j.ejogrb.2005.11.036
- Hill GB. The microbiology of bacterial vaginosis. American Journal of Obstetrics and Gynecology. 1993;169(2):450-454. doi:10.1016/0002-9378(93)90339-K
- Gilbert NM, O’Brien VP, Lewis AL. Transient microbiota exposures activate dormant Escherichia coli infection in the bladder and drive severe outcomes of recurrent disease. Mobley HLT, ed. PLoS Pathog. 2017;13(3):e1006238. doi:10.1371/journal.ppat.1006238
- Wiesenfeld HC, Hillier SL, Krohn MA, Landers DV, Sweet RL. Bacterial Vaginosis Is a Strong Predictor of Neisseria gonorrhoeae and Chlamydia trachomatis Infection. CLIN INFECT DIS. 2003;36(5):663-668. doi:10.1086/367658
- Thorsen P, Vogel I, Olsen J, et al. Bacterial vaginosis in early pregnancy is associated with low birth weight and small for gestational age, but not with spontaneous preterm birth: A population-based study on Danish women. The Journal of Maternal-Fetal & Neonatal Medicine. 2006;19(1):1-7. doi:10.1080/14767050500361604
- Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. American Journal of Obstetrics and Gynecology. 1988;158(4):819-828. doi:10.1016/0002-9378(88)90078-6
- Bradshaw CS, Morton AN, Hocking J, et al. High Recurrence Rates of Bacterial Vaginosis over the Course of 12 Months after Oral Metronidazole Therapy and Factors Associated with Recurrence. J INFECT DIS. 2006;193(11):1478-1486. doi:10.1086/503780
- Marrazzo JM, Koutsky LA, Eschenbach DA, Agnew K, Stine K, Hillier SL. Characterization of Vaginal Flora and Bacterial Vaginosis in Women Who Have Sex with Women. J INFECT DIS. 2002;185(9):1307-1313. doi:10.1086/339884
- Calzolari E, Masciangelo R, Milite V, Verteramo R. Bacterial vaginosis and contraceptive methods. International Journal of Gynecology & Obstetrics. 2000;70(3):341-346. doi:10.1016/S0020-7292(00)00217-4
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
- March 28, 2024
Updated
Check out Happy V Pre+Pro for a product made with clinically proven vaginal probiotic strains proven to alleviate the symptoms of BV.
- A-
- A+
Check out Happy V Pre+Pro for a product made with clinically proven vaginal probiotic strains proven to alleviate the symptoms of BV.