- Bacterial vaginosis is caused by an overgrowth of bacteria, the most common being Gardnerella vaginalis.
- This overgrowth of bacteria can cause inflammation, which can result in mild cramping.
- Generally, BV-related cramps present as a low, persistent ache and may be accompanied by other symptoms like thin, grayish vaginal discharge.
- If you suspect you have a vaginal infection, make an appointment with your healthcare provider. If you experience severe abdominal pain, seek immediate medical care.
- After completing treatment for BV, consider lifestyle changes such as practicing safe sex, wearing cotton underwear, and taking daily probiotics to prevent recurrence.
Occasional cramps come with the territory of being a proud vagina owner. But if you are experiencing cramping that doesn’t align with your menstrual cycle and doesn’t quite feel like the period cramps you’re used to, you are probably wondering what’s going on and if this cramping is NBD or a sign of something larger.
Here, we’re going to be diving into the link between vaginal infections and cramping. Specifically, we’ll be talking about bacterial vaginosis or BV and if it ever contributes to uterine cramps and general abdominal pain. But before we can dive into the potential symptoms of BV, we have to understand what BV is.
Understanding Bacterial Vaginosis (BV)
Bacterial vaginosis is a vaginal infection caused by an overgrowth of bad bacteria. According to CDC data, BV is actually the most common vaginal infection among women ages 15-44, affecting over 21 million women every year in the United States alone.
There are several types of bacteria that can cause BV, but the main culprit is a bacteria called Garderella vaginalis. The interesting thing about G. vaginalis is that it is actually part of most healthy vaginas. So why does G. vaganalis sometimes cause infections and other times it doesn’t? It really has to do with the overall health of your vaginal microbiome.
Healthy vaginal microbiomes contain a probiotic called Lactobacillus. Lactobacillus releases lactic acid that kills bad bacteria before it can cause infection1. However, if something has disrupted the vaginal microbiome and impacted the amount of Lactobacillus living in it, there are less good bacteria to fight off the bad, meaning previously benign bacteria like Gardnerella vaginalis have the opportunity to grow rapidly and overtake the microbiome, causing infection.
We will be getting into the possible symptoms of BV a bit later, but it’s important to know that as prevalent as BV is, it can also be easily confused for other infections, including urinary tract infections and vaginal yeast infections. This is why it’s so important to see your doctor if you ever suspect a vaginal infection. Only they will be able to confirm your diagnosis with 100% certainty.
How BV Relates to Cramping and Lower Abdominal Pain
Okay, now that we’ve established what BV is, let’s get to the answer you came for: does BV cause cramping? Well… yes and no.
BV doesn’t directly cause cramps, but the overgrowth of bacteria within the vagina can lead to inflammation of the vaginal tissue, and the inflammation can lead to cramping sensations or dull pain in the lower abdomen. However, the sensation associated with BV-related cramps is a bit different than the cramps typically associated with menstruation. We’ll get into the differences next.
Recognizing the Symptoms of BV and Associated Cramps
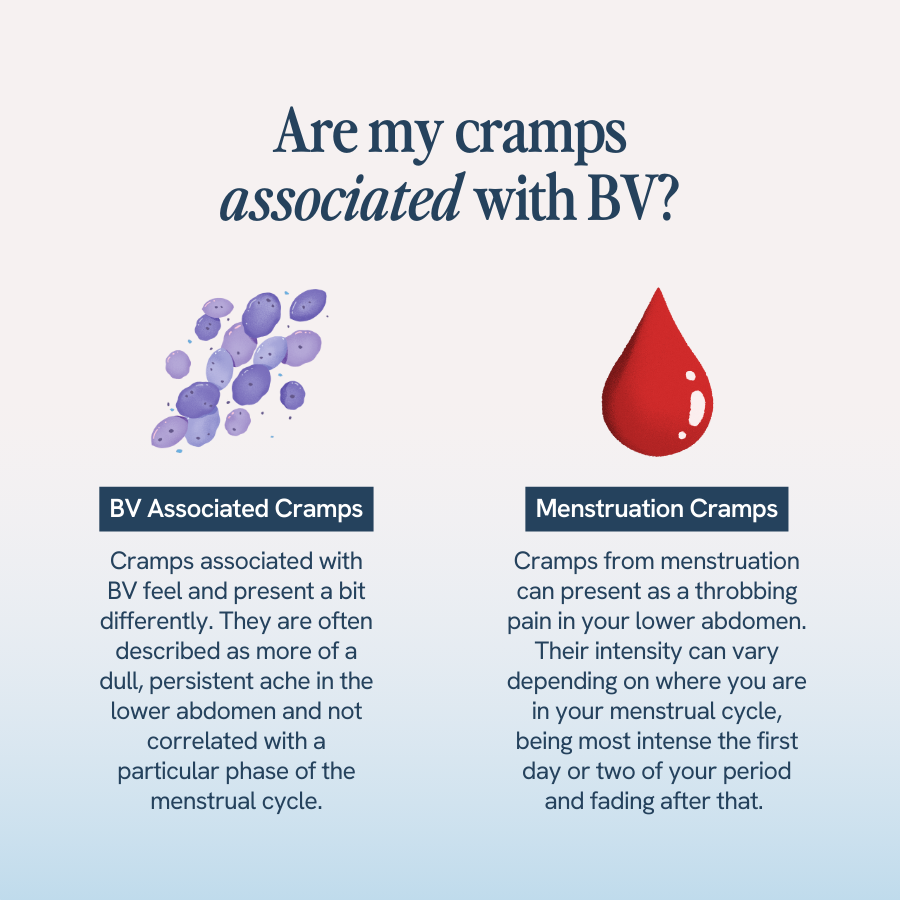
If you have a vagina, chances are, you are probably familiar with the cramps associated with menstruation. They are a throbbing or cramping feeling in your lower abdomen, with a pain level ranging from “minor nuisance” to “total life disruption.” Their intensity can also vary depending on where you are in your menstrual cycle, being most intense the first day or two of your period and fading after that.
Cramps associated with BV feel and present a bit differently. They are often described as more of a dull, persistent ache in the lower abdomen and not correlated with a particular phase of the menstrual cycle. They are also often noticed in tandem with other BV symptoms, which we’ll get into next. But before we dive into that, we do want to say that if you ever notice you are having any kind of severe or prolonged pain in the abdomen, that should never go ignored and always warrants medical evaluation, whether that’s a same-day trip to your doctor, an urgent care visit, or even a trip to the ER.
Other Symptoms Accompanying BV and Cramps

While cramps can be associated with BV, they are generally not the only symptom. The most common symptom of BV is an increase of vaginal discharge that is also thin, gray-ish, and accompanied by a strong or “fishy” odor2. Many people also report that this “fishy” odor gets worse immediately after sex.
Other symptoms of BV include:
- Pain, itching, or burning in the vagina
- Burning during urination
- Itching around the outside of the vagina3
If you are experiencing cramps in conjunction with any of these symptoms, that’s a sign you need to your gynecologist or other healthcare provider to get tested for BV. What will that appointment look like? Keep reading.
Diagnosis and Treatment of BV Causing Cramps
If you go to the doctor because of BV-like symptoms, your doctor will not make a diagnosis based on your symptoms alone. They will generally perform a pelvic exam and analyze samples of vaginal fluid to see exactly what’s going on.
If they do determine you have BV and not an infection with similar symptoms like a UTI or Trichomoniasis, they will likely prescribe you antibiotics, with the two most common being metronidazole and clindamycin.
And while antibiotics may be necessary to clear an active infection (and help you get rid of those uncomfortable cramps!), they are not without side effects, one of the biggest being that they not only kill the infection-causing bacteria but also that good Lactobacillus bacteria. Without healthy levels of Lactobacillus, you are more prone to secondary infections, like vaginal yeast infections, following antibiotics.
This is where a daily probiotic supplement like Happy V’s Prebiotic + Probiotic can make a real difference. Happy V’s Prebiotic + Probiotic is doctor-formulated to include the most important strains of Lactobacillus responsible for maintaining vaginal health. By taking them in conjunction with antibiotics, you are replenishing your levels of healthy bacteria daily to not only fight off future BV infections but other secondary infections like vaginal yeast infections.
Complications of Untreated BV
If you’re thinking, “I don’t have time for a doctor’s appointment, and the cramps really aren’t that bad anyway,” let us stop you right there. Because the worst thing you can do for your health in the short- and long-term is to ignore BV symptoms.
Though BV is incredibly common and highly treatable, it can lead to much bigger health consequences if left untreated, including pelvic inflammatory disease (PID) and infertility. In pregnant women, untreated BV can also increase your risk of preterm labor and low birth weight.
We know everyone is super busy these days. But your health is too important to put off or ignore.
Preventive Measures for BV and Associated Cramps
So antibiotics can help clear an active BV infection and get rid of those uncomfortable cramps. But how can you prevent those cramps from coming back? There are a few key lifestyle changes you want to make, including:
- Practicing safe sex. Condoms don’t exactly have a reputation for being sexy… unless you think health is sexy. Condoms can protect you from being exposed to any infection-causing bacteria that may be living on your partner’s genitals, including bacteria that lead to BV.
- Wearing cotton, breathable underwear. Synthetic fabrics like nylon trap moisture and aid in bacteria overgrowth. Instead, opt for natural cotton underwear to prevent moisture build-up.
- Maintain good vaginal hygiene. This includes things like not douching, washing your vagina using only warm water and unscented soap, and wiping from front to back after using the bathroom.
- Taking daily probiotics. Happy V’s Prebiotic + Probiotic isn’t just a way to mitigate antibiotic side effects, it is a proven way you can maintain everyday vaginal health and ensure your body has the levels of Lactobacillus it needs to fight off a range of infections.
- Bacterial Vaginosis (BV): A common vaginal infection caused by an overgrowth of certain bacteria, particularly Gardnerella vaginalis, disrupting the vaginal microbiome.
- Vaginal Microbiome: The community of microorganisms that naturally reside in the vagina, including beneficial bacteria like Lactobacillus.
- Lactobacillus: A type of probiotic bacteria found in the vagina that helps maintain a healthy acidic environment, protecting against infections like BV.
- Inflammation: A localized physical condition where part of the body becomes reddened, swollen, hot, and often painful, typically as a response to infection or injury.
- Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, usually caused by sexually transmitted bacteria spreading from the vagina to the uterus, fallopian tubes, or ovaries.
- Preterm Labor: The onset of labor before the 37th week of pregnancy.
- Antibiotics: Medications used to treat bacterial infections by either killing the bacteria or stopping their growth.
- Probiotics: Live microorganisms that provide health benefits when consumed in adequate amounts, often referred to as “good” or “friendly” bacteria.
- Vaginal Yeast Infection: A fungal infection caused by an overgrowth of yeast in the vagina, often occurring after antibiotic use.
- UTI (Urinary Tract Infection): An infection in any part of the urinary system, including the kidneys, bladder, ureters, or urethra.
- Trichomoniasis: A sexually transmitted infection (STI) caused by the parasite Trichomonas vaginalis.
- Gardnerella vaginalis: A type of bacteria commonly associated with bacterial vaginosis (BV) when its overgrowth disrupts the vaginal microbiome.
- Bacterial Vaginosis (BV) – Fact Sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm Accessed April 26, 2024.
- Mashatan N, Heidari R, Altafi M, Amini A, Ommati MM, Hashemzaei M. Probiotics in vaginal health [published correction appears in Pathog Dis. 2023 Jan 17;81:]. Pathog Dis. 2023;81ftad012. doi:10.1093/femspd/ftad012
- Meena V, Bansal CL. Study to Evaluate Targeted Management and Syndromic Management in Women Presenting with Abnormal Vaginal Discharge. J Obstet Gynaecol India. 2016;66(Suppl 1):534-540. doi:10.1007/s13224-016-0879-x
- Bacterial vaginosis – STI treatment guidelines. Centers for Disease Control and Prevention. July 22, 2021. Accessed May 2, 2024. https://www.cdc.gov/std/treatment-guidelines/bv.htm.
- A-
- A+






