- Bacterial vaginosis, or BV, is a vaginal infection caused by the overgrowth of harmful bacteria in the vaginal environment.
- Bacterial vaginosis symptoms may include an increase in vaginal discharge (with a characteristically fishy smell), itchiness in the vaginal area, or a burning sensation around the vagina while urinating.
- Whenever you have intercourse with a sex partner, your vagina’s bacteria levels are disrupted by new bacteria from this partner, which can cause BV. However, many sexual and non-sexual factors can cause BV, and some who have never had sex develop BV.
Developing a vaginal condition after having sex can make you very worried. If you’re still with your regular partner, you may wonder if they’re cheating on you. If you’re with a new partner, you might be concerned that your symptoms are the result of a sexually transmitted infection (STI). You might even wonder if your abnormal discharge or vaginal discomfort is an early sign of pregnancy!
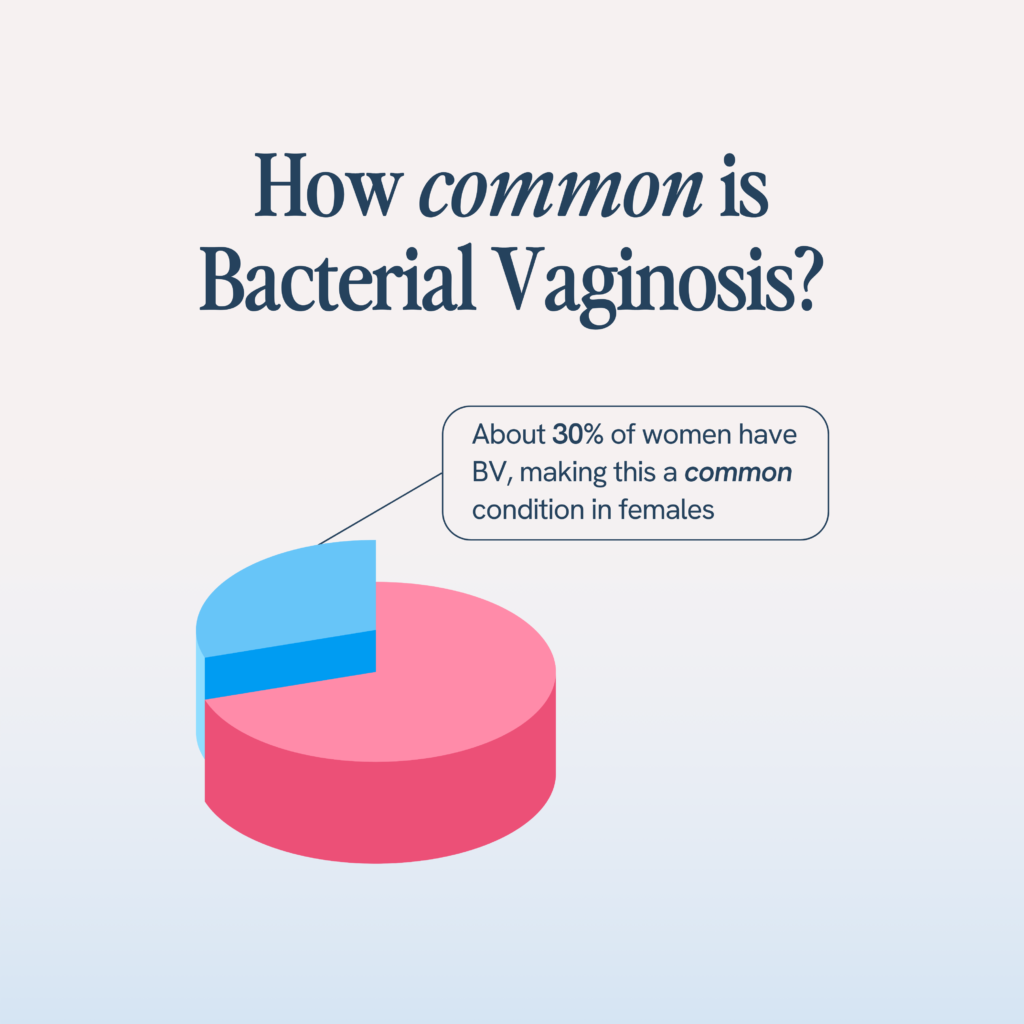
In many cases, common symptoms in the vagina, like itchiness, redness, or unusual vaginal discharge, are a result of an imbalance of bacteria causing bacterial vaginosis, or BV. BV isn’t an STI, but it’s still a serious medical condition that requires treatment. BV is a common condition in females—about 30% of women have BV, although only half of those have symptoms. (1)
If you’re struggling with BV, you probably want to know how to prevent its occurrence. Research shows that sex can trigger a bacterial vaginosis infection, even though BV is not an STI. In this article, we’ll discuss what BV is, why some people get BV after sex, the risk factors for developing BV, potential complications arising from BV, and tips for a healthy vagina.
What Is BV?
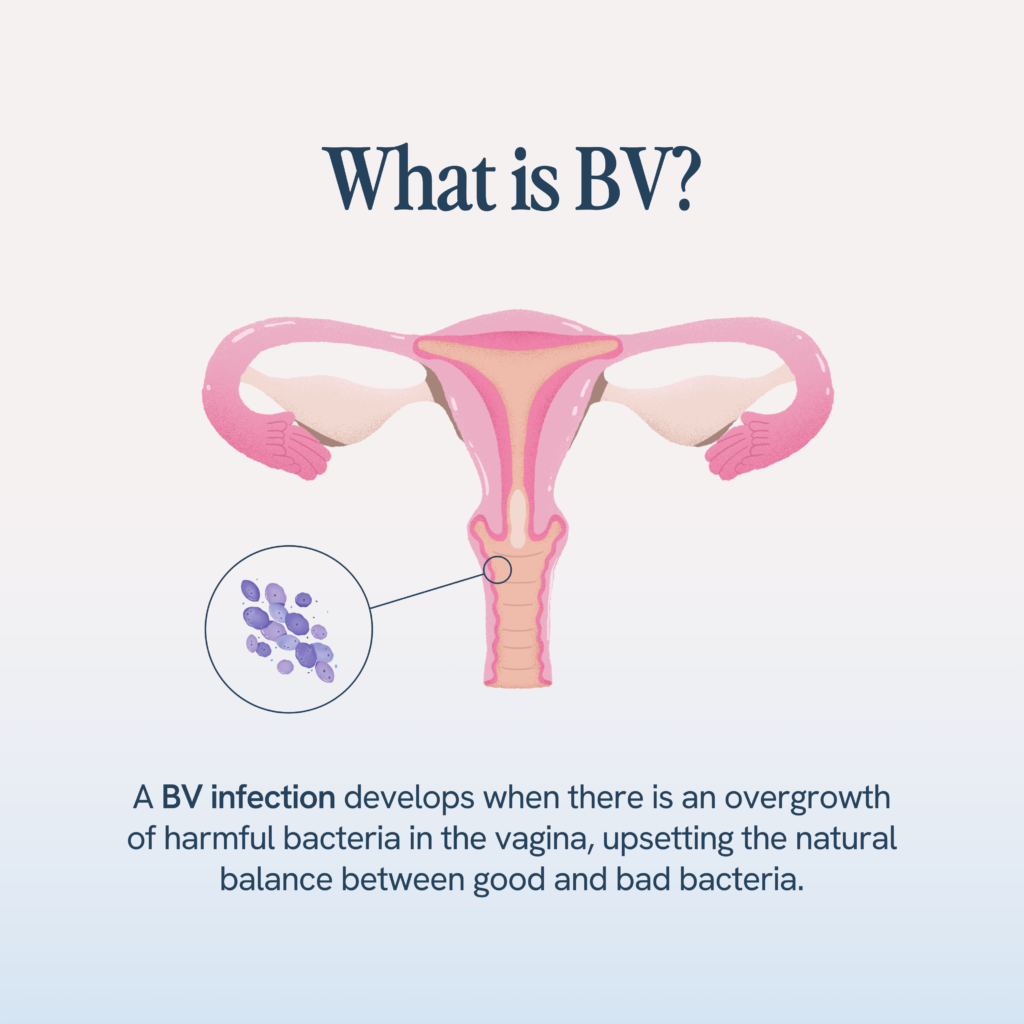
Bacterial vaginosis, or BV, is a vaginal infection caused by the overgrowth of harmful bacteria in the vaginal environment. The vagina contains a natural balance of bacteria, called vaginal lactobacilli, that help balance vaginal acidity levels and prevent the overgrowth of bacteria that can cause infection. When this normal balance becomes disrupted, BV can develop.
BV is not an STI because the bacteria that cause BV are naturally present in the vagina—a BV infection is triggered when the balance between good and bad bacteria in the vagina is disrupted. An STI, however, is caused by the presence of abnormal bacteria in the vagina.
Usually, the self-cleaning abilities of your vagina allow it to rid itself of bad bacteria on its own. However, if the infection is too severe, treatment from a healthcare professional may be required to prevent the infection from recurring. Over 50% of women who experience a BV infection will experience a recurrence of symptoms within 1 year. (2) If left untreated, BV can trigger other medical problems including pregnancy complications, like preterm delivery or a low-birth-weight baby, and an increased risk of developing an STI, HIV, or pelvic inflammatory disease.
What Are the Symptoms of BV?
BV is characterized by an increased vaginal acidity and a host of embarrassing and uncomfortable vaginal symptoms.
According to the CDC, more than 85% of women with BV are asymptomatic. (3) However, those that do experience bacterial vaginosis symptoms may notice an increase in vaginal discharge (with a characteristically fishy smell), itchiness in the vaginal area, or a burning sensation around the vagina while urinating.
The vaginal discharge exhibited by women with BV is quite unusual. It typically is characterized by:
- Consistency: Thin
- Color: Gray or white discharge
- Smell: Sharp and pungent vaginal odor; often defined as a strong fish-like odor
- Cramps – such as a dull, persistent ache in the lower abdomen, distinct from typical menstrual cramps
What Causes Bacterial Vaginosis?
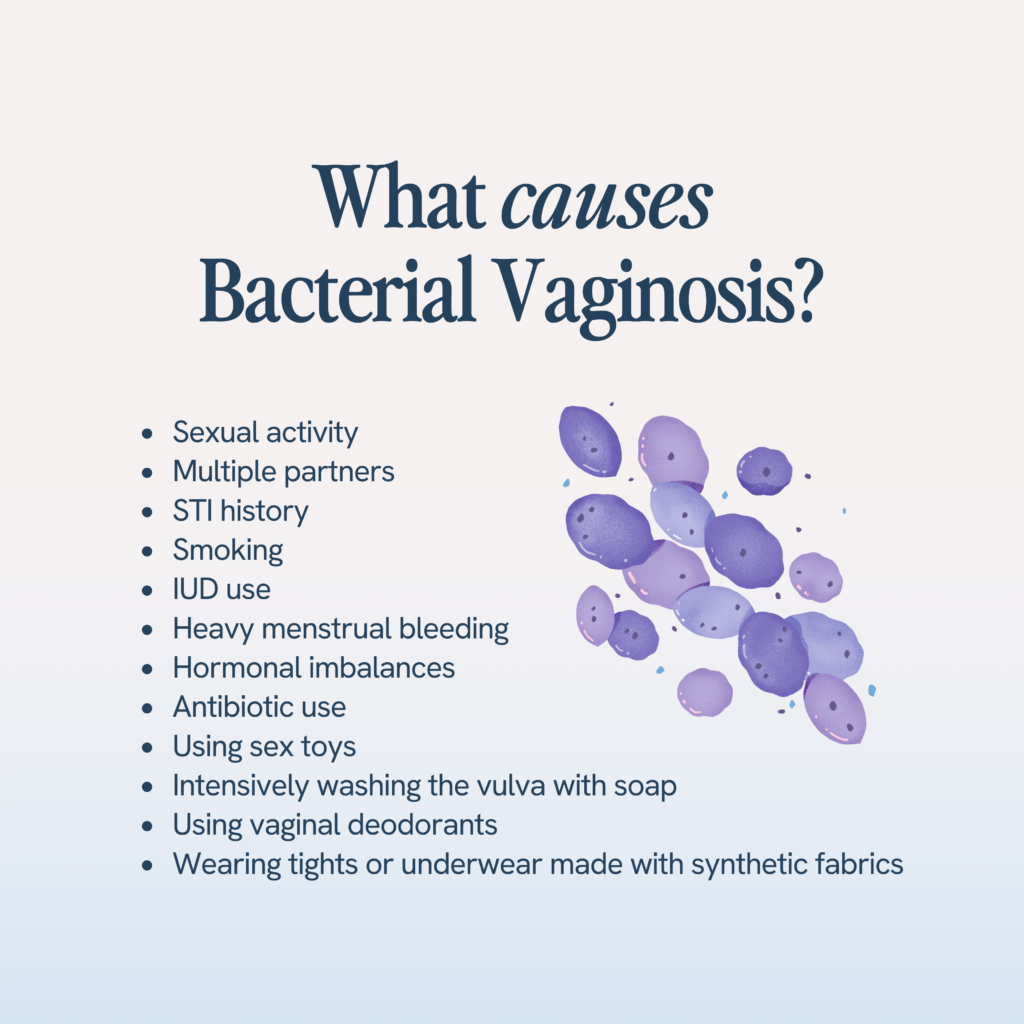
While the exact cause of BV is unknown, women characterized by the following sexual and non-sexual factors are the most likely to develop BV. The prevalence of BV is higher among women of childbearing age, and those with the highest likelihood of getting BV are women who: (4)
- Are sexually active, especially women who have sex with women. Bacterial vaginosis can occur after having sex with both male and female partners, but women with a female sex partner are the most likely to develop BV
- Change their sexual partners regularly or have more than one sexual partner
- Have a history of STIs
- Smoke or drink excessively
- Use an intrauterine contraceptive device (IUD)
- Experience heavy menstrual bleeding
- Take perfumed bubble baths or douche (5)
- Have hormonal imbalances after puberty, pregnancy, or menopause. Pregnant women are more likely to get BV than non-pregnant women (6)
- Have an imbalance in their vaginal pH
- Are on antibiotic treatment. Frequent usage of antibiotics tends to kill good vaginal bacteria and predisposes females to BV or other infections such as candida or thrush
Additionally, any activity that lowers your vaginal pH can disrupt your body’s balance of healthy bacteria and harmful bacteria and cause reproductive health issues, including:
- Use of sex toys
- Intensively washing the vagina with soap. Strong detergents and scented soaps can disrupt the vaginal pH, but even washing your vagina with water can cause an overgrowth of bacteria
- Using vaginal deodorant
- Wearing nylon tights or thongs for long periods
An activity that triggers BV in one person might not necessarily cause it in another. However, if you’re noticing signs of bacterial vaginosis, particularly vaginal discomfort and the characteristic smell, it’s important to contact your healthcare provider to get treatment.
Why do I Keep Getting BV After Sex?
Now you’re probably wondering…if BV isn’t an STI, why do so many women get it after having sex?
The female genitals are home to many types of bacteria, including anaerobic bacteria and lactobacilli (lactic acid-producing bacteria), which maintain the normal pH balance of the vagina. Whenever there is an imbalance of these bacteria causing the number of anaerobic bacteria to increase and the number of lactobacilli to decrease, the vagina may develop bacterial vaginosis.
Whenever you have intercourse with a new sex partner, your vagina’s bacteria levels are disrupted by new bacteria from this partner, which can cause BV. Men can’t get infected with BV, even if they’re housing BV-associated bacteria that causes it, so if you have sex with a new male partner, their bacteria may trigger an infection. Since so many women don’t experience symptoms from BV, you can also get BV from a same-sex partner with asymptomatic BV.
If you’ve been with your current partner for a while and recently got BV, you might be concerned that your partner is cheating on you. Before you jump to conclusions, remember that BV can be triggered by many different activities that disrupt the vaginal microbiome. In fact, you can get BV, even if you’ve never had sex! Recurring BV with the same partner is (unfortunately) quite normal, but a healthcare provider can help you get past the infection.
Complications of Bacterial Vaginosis
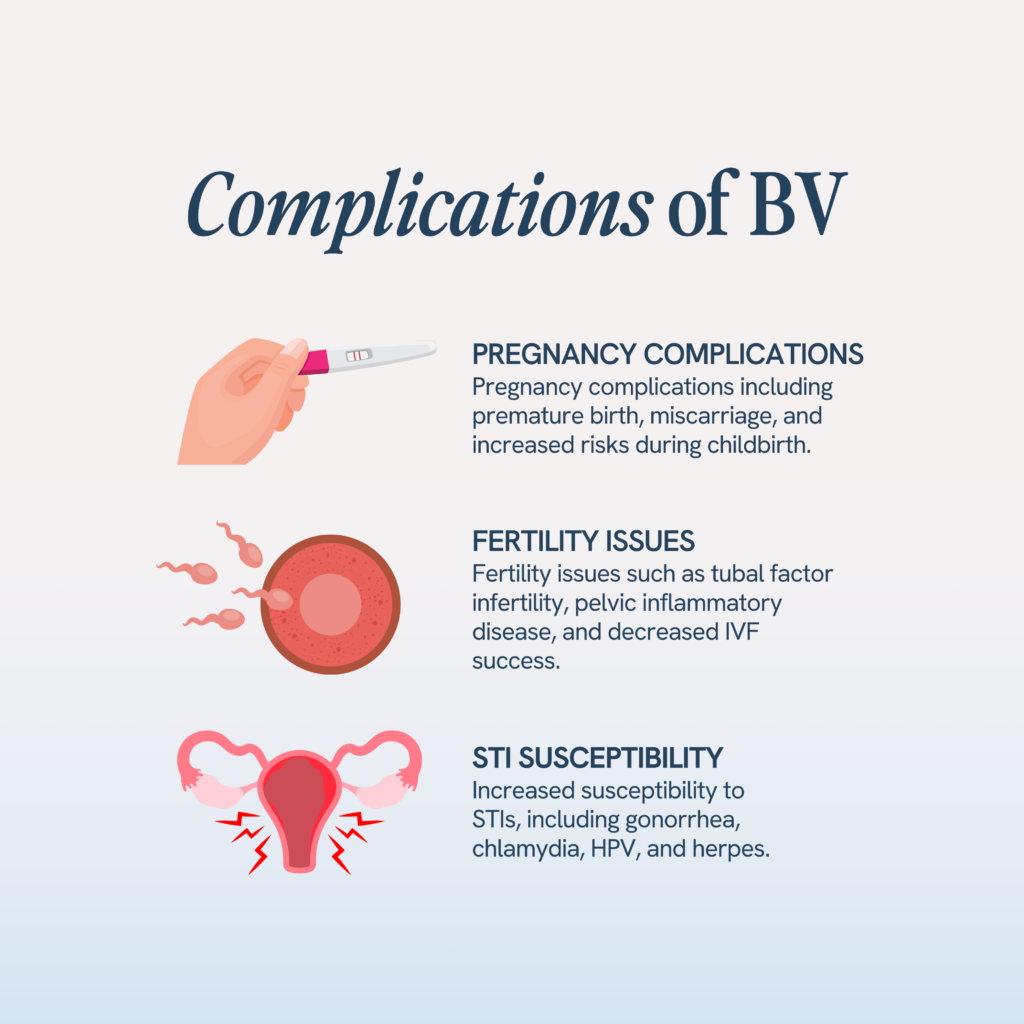
By itself, BV is not a serious health issue, but it can lead to many medical complications including common infections such as vaginal yeast infections, chlamydia, or vaginitis. (7)
General Health Complications
Having BV can increase the risk of developing an STI such as:
- Gonorrhea
- Chlamydia
- Human papillomavirus
- Herpes
Additionally, BV increases the susceptibility to getting HIV and increases the chances of having a post-surgical infection after a procedure like a hysterectomy or abortion.
Pregnancy Complications
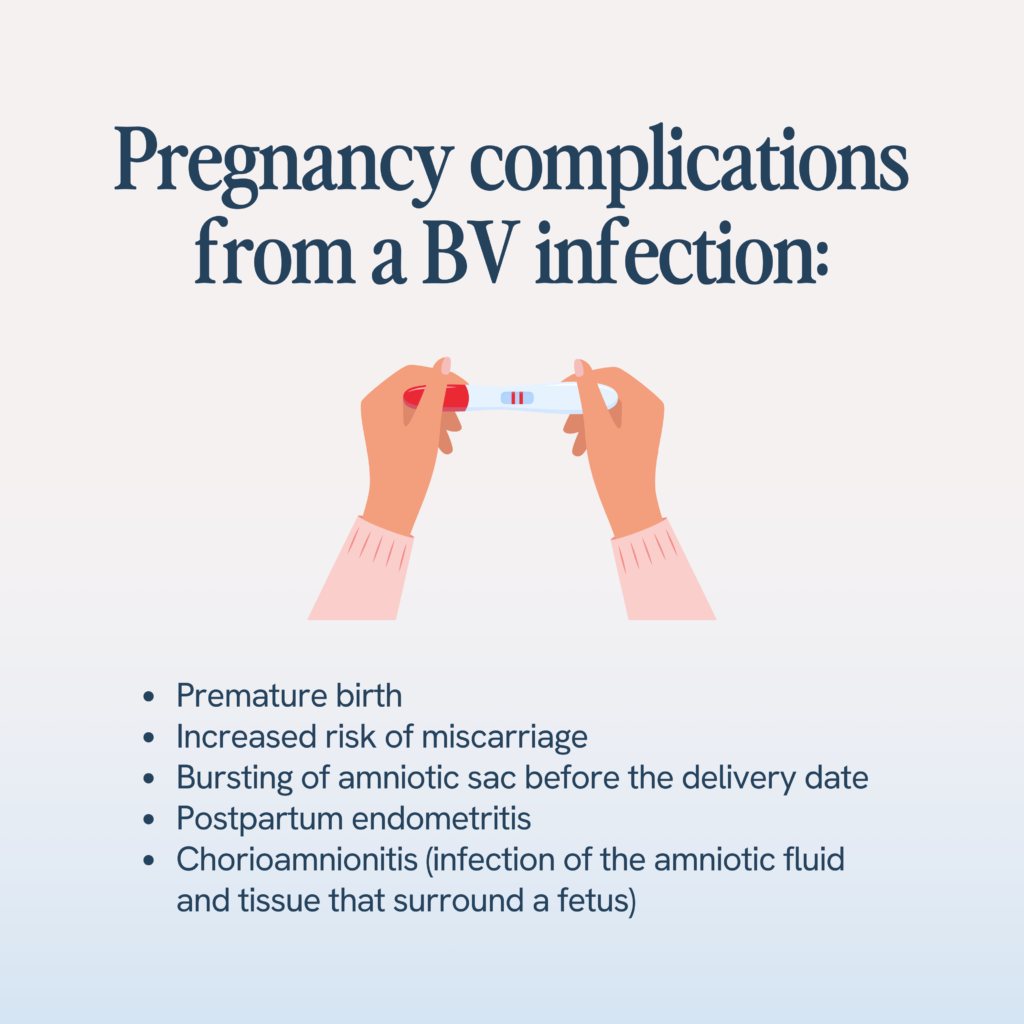
BV can cause some pregnancy complications, so it’s particularly important to get treatment if you suspect a BV infection while pregnant. Complications may include:
- Premature birth (birth before 37 weeks of pregnancy)
- Increased risk of miscarriage
- Bursting of amniotic sac before the delivery date
- Postpartum endometritis, which causes inflammation or irritation of the uterus lining after delivery
- Chorioamnionitis, which causes inflammation of the layers surrounding the fetus. Chorioamnionitis also increases the likelihood of having a preterm birth or a child who develops cerebral palsy
Fertility Complications
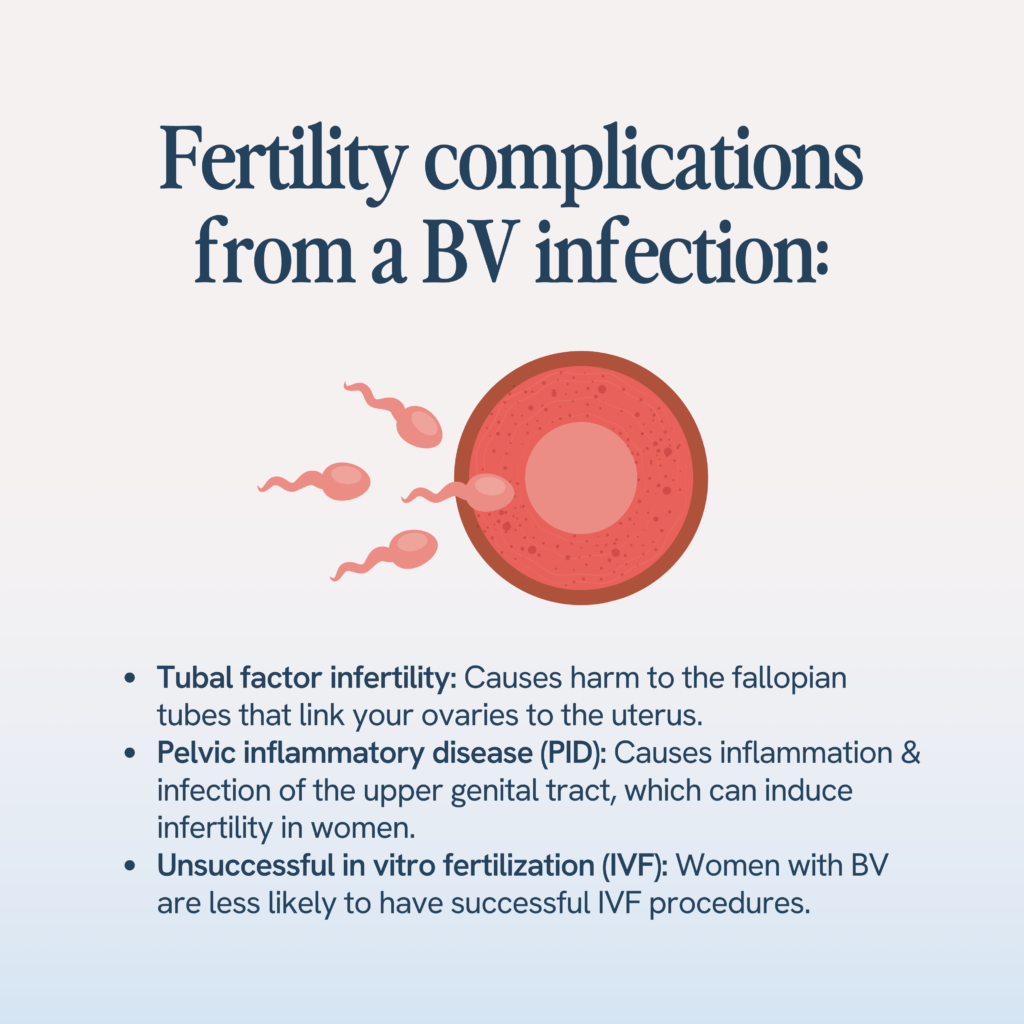
Women struggling with fertility are three times as likely to have BV than fertile women. (8) BV can worsen fertility struggles by causing:
- Tubal factor infertility. This type of infertility causes harm to the fallopian tubes that link your ovaries to the uterus.
- Pelvic inflammatory disease. This condition causes inflammation and infection of the upper genital tract, which can induce infertility in women.
- Unsuccessful in vitro fertilization (IVF). Women with BV are less likely to have successful IVF procedures.
Treatment for Bacterial Vaginosis
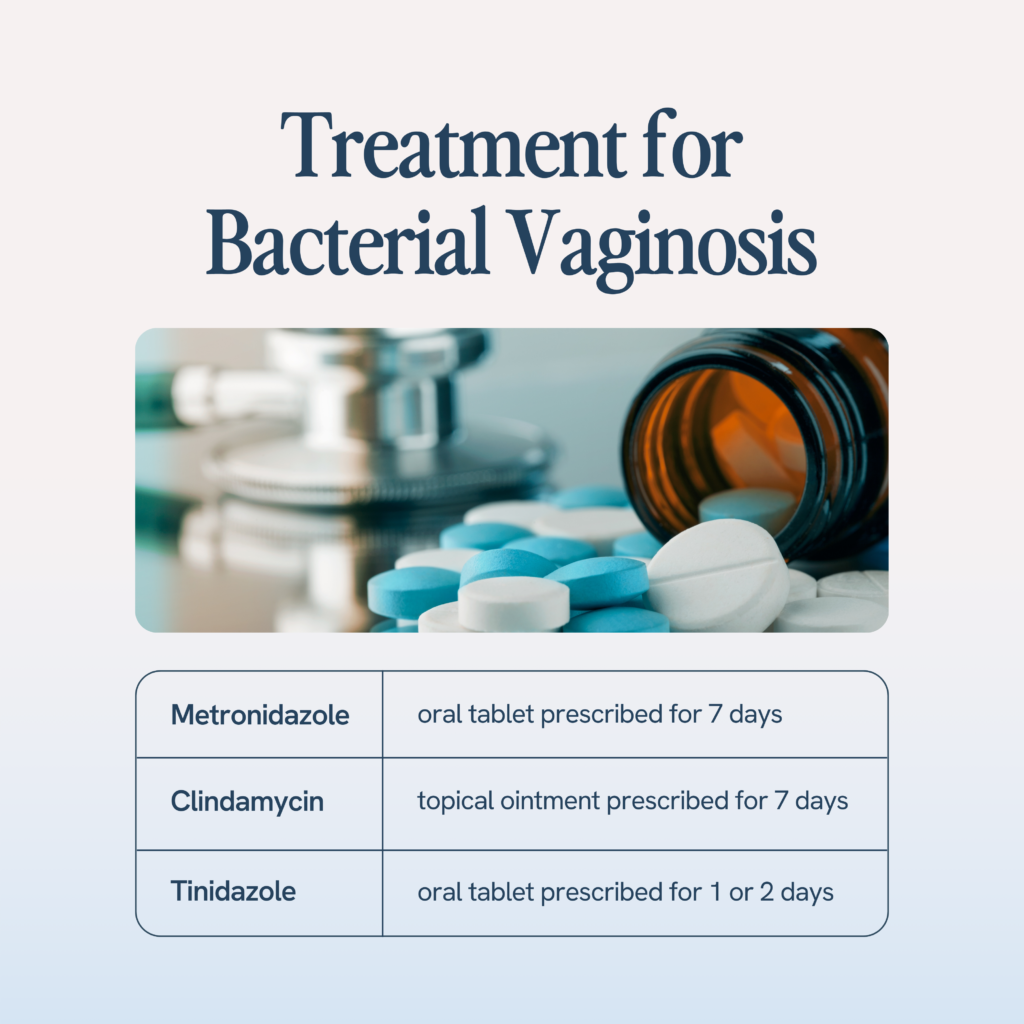
Often, BV doesn’t require active treatment and may clear up on its own. However, leaving it untreated might increase the risk of a recurrence of symptoms if the infection does not completely go away on its own.
If a healthcare provider recommends treatment for your BV infection, it’s important to follow their instructions precisely to avoid a persistent infection. Antibiotics are highly effective against BV. (9) Some antibiotics that are commonly given in BV are:
- Metronidazole, an oral tablet prescribed for 7 days
- Clindamycin, a topical ointment prescribed for 7 days
- Tinidazole, an oral tablet prescribed for 1 or 2 days
Even after taking these medications, many women experience recurrent symptoms within the first 12 months after treatment. To treat recurrent bacterial vaginosis, your doctor might prescribe you an extended course of oral metronidazole or metronidazole ointment for as little as 10 days or up to 3 months to completely rid your body of the infection.
How To Maintain Your Sexual Health and Prevent a BV Infection
Lifestyle modifications are key to preventing BV from occurring in the first place. To prevent BV:
- Use a combined oral contraceptive drug instead of intrauterine devices for birth control
- Have protected sex. Using condoms can help prevent BV occurrence, although it might not prevent a recurrent symptoms once you are infected with BV (10)
- Take probiotics for vaginal health. Probiotics help boost your body’s lactobacilli levels, which can prevent BV from occurring.
- Avoid douching
- Wear breathable panties and bottoms
- Don’t overuse antibiotics
Our Happy V® Prebiotic + Probiotic was created for anyone who is experiencing symptoms related to Bacterial Vaginosis and Yeast Infections. Eliminate the odor, itch, gut bloating, and other symptoms.
Why do I Get BV After Sex: The Bottom Line
BV isn’t an STI—it’s caused by an overgrowth of anaerobic bacteria which disrupts the vaginal pH, resulting in uncomfortable BV symptoms. Many sexual and non-sexual factors can cause this bacterial overgrowth, and the key to avoiding BV is to practice safe sex practices and great vaginal hygiene.
Happy V’s targeted BV products are designed to keep you free from the discomfort and embarrassment associated with BV. Our liquid chlorophyll drops are a natural BV odor remedy to help you manage that characteristic smell, and our cranberry pills for BV help naturally rebalance the vaginal microbiome by making it difficult for anaerobic bacteria to adhere to the vaginal wall and cause an overgrowth.
If you’re struggling with recurrent BV or other uncomfortable vaginal symptoms, it’s important to seek treatment from a healthcare provider. Since BV can increase your risk for serious medical conditions, like HIV, pregnancy and fertility complications, and STIs, proper treatment is vital to maintaining your reproductive health.
- https://pubmed.ncbi.nlm.nih.gov/17621244/#:~:text=Results%3A%20The%20prevalence%20of%20BV,with%20BV%20reported%20vaginal%20symptoms
- https://www.liebertpub.com/doi/10.1089/jwh.2018.7383#:~:text=Abstract,of%20treatment%20for%20incident%20disease.
- https://www.ncbi.nlm.nih.gov/books/NBK459216/
- https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm
- https://www.womenshealth.gov/a-z-topics/douching
- https://americanpregnancy.org/healthy-pregnancy/pregnancy-complications/bacterial-vaginosis-during-pregnancy/
- https://www.ncbi.nlm.nih.gov/books/NBK459216/
- https://americanpregnancy.org/getting-pregnant/bacterial-vaginosis-and-fertility/#:~:text=Bacterial%20Vaginosis%20is%20three%20times,to%20sperm%20and%20vaginal%20cells
- https://www.ncbi.nlm.nih.gov/books/NBK298830/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5161033/#:~:text=Consistent%20condom%20use%20was%20associated%20with%20reduced%20BV%20prevalence%20at,occurence%2C%20but%20not%20BV%20recurrence.
- A-
- A+