- Yeast infections are caused by an overgrowth of fungi, and this overgrowth can cause symptoms like cottage cheese-like vaginal discharge and inflammation or irritation of the genital area.
- If you are experiencing severe or recurrent yeast infections, the inflammation can impact your menstrual cycle and possibly delay your period.
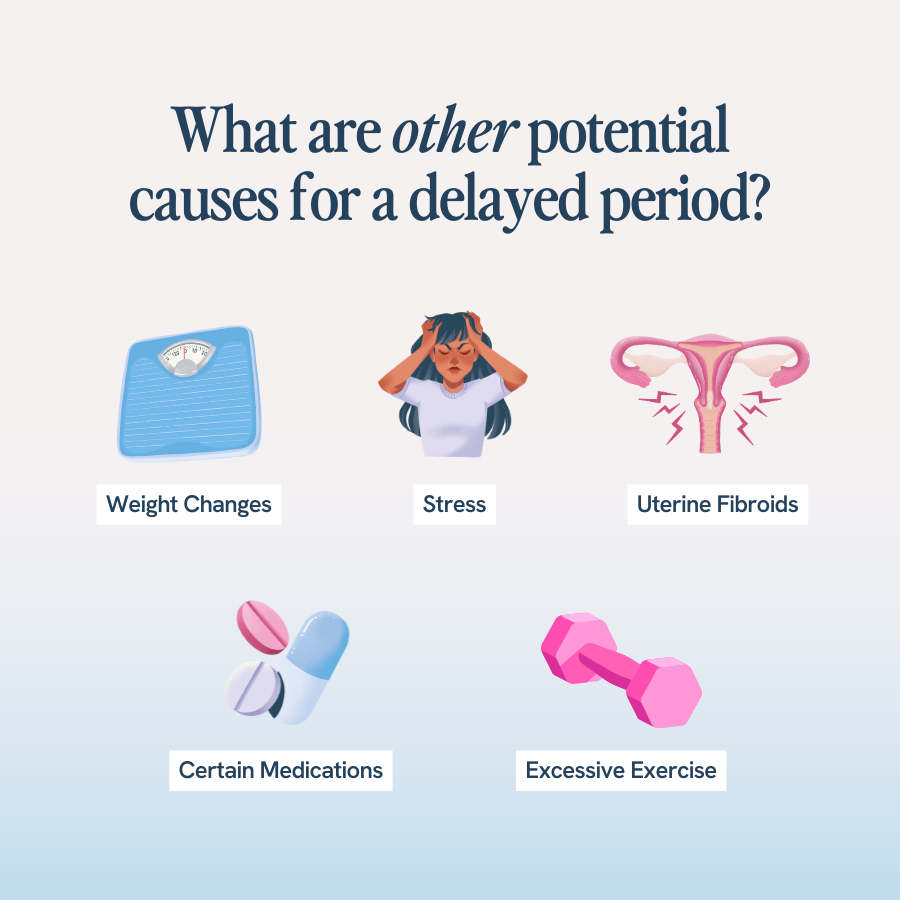
- Other causes of delayed periods include stress, certain medications, excessive exercise, and significant weight changes.
- If you ever suspect you have a yeast infection, especially one that is delaying your period or causing unusual bleeding, make an appointment with your provider.
- If you are experiencing recurrent yeast infections, ask your doctor if daily probiotics could be the solution you need to restore your vaginal microbiome and end the cycle of infection.
Yeast infections — and the symptoms that come along with them — are pretty disruptive. But can yeast infections actually disrupt your menstrual cycle and delay your period?
The answer to this question isn’t so straightforward, but it’s important to understand how yeast infections can — and can’t — interact with your menstrual cycle. After all, sexual health is not just about reproduction; it’s an important indicator of your overall wellness.
Understanding Yeast Infection
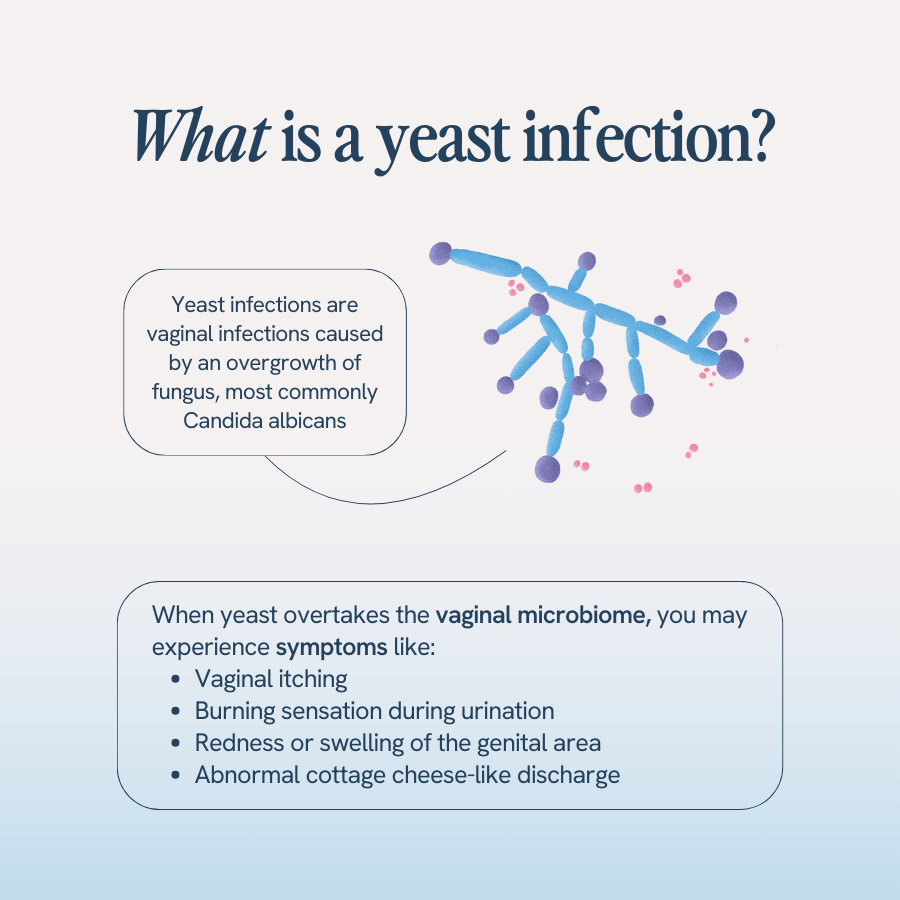
Before we can get into how yeast infections might delay menstruation, let’s talk about what they are. Yeast infections are vaginal infections caused by an overgrowth of fungus, most often the fungus Candida albicans. The Candida fungus is what gives yeast infections their alternate names, particularly candidiasis and vulvovaginal candidiasis.
When yeast overtakes the vaginal microbiome, you experience symptoms like:
- Vaginal itching
- Burning sensation during urination
- Redness or swelling of the genital area
- Abnormal vaginal discharge, which most people describe as “cottage cheese-like”
- Sores – typically painful and raw
- Bumps – may feel firm and are often less painful.
This abnormal vaginal discharge is typically considered the hallmark symptom of a yeast infection. But what about a delayed period? Are yeast infections known for that, too? Keep reading!
Yeast Infection and Your Menstrual Cycle
By now, you are probably more than familiar with your menstrual cycle, which for most people occurs every 28 days but can occur anywhere between 21 and 35 days.
The timing of menstruation (aka your period) has to do with the timing of certain hormonal fluctuations that regulate ovulation, thicken the uterine lining, and, when pregnancy doesn’t occur, shed the uterine lining.
Yeast infections can’t directly impact your menstrual cycle, but they certainly disrupt the normal vaginal environment, which can lead to other health consequences.
Can Yeast Infection Delay Your Period?
So what are these “health consequences” we just mentioned? Can yeast infections delay your period?
In a roundabout way, yes. Yeast infections themselves don’t delay your period, meaning delayed periods are not a direct symptom of yeast infections. But yeast infections, especially recurrent ones, can cause inflammation and irritation in the vagina that can potentially affect the processes of the menstrual cycle. So, if you have been struggling with severe or recurrent yeast infections and are noticing your periods are becoming irregular or delayed, it may be due to ongoing inflammation.
Yeast Infection before Period: What to Know
Many women who experience chronic or recurrent yeast infections report that they always seem to get their yeast infections right before their period. Can this be true? Well, yes! Those hormonal fluctuations we mentioned earlier? They include drops in your estrogen levels, and with lower levels of estrogen, your vaginal pH may become imbalanced. And vaginal pH is important because it helps to kill bad microbes — like yeast — before they can multiply and cause infection.
So, essentially, in the days leading up to your period, your changing hormones do leave you more vulnerable to vaginal infections like yeast infections since your vaginal pH may not be able to fight off yeast as efficiently as it does other times of the month. Luckily, there is a natural way to help boost your immunity to vaginal infections. We’ll get into what that is in just a bit!
Other Potential Causes of Delayed Period
Though there may be a link between the inflammation from recurrent yeast infections and delayed periods, more research is needed to understand this link and how long a yeast infection can actually delay a period.
So if your period is more than just a day or two late and you are wondering, “Well, how long can infection delay my period, anyway?” there may actually be something else at play.
Of course, if you ever expect your yeast infections are severe enough that they are messing with your menstrual cycle, you should make an appointment with your doctor. But know that stress, certain medications, excessive exercise, uterine fibroids, and significant weight changes have all been shown to impact your menstrual cycle, and your doctor should help you pursue all possible causes.
Diagnosis and Treatment Options for Yeast Infection
When you do go to discuss a potential yeast infection with your doctor, they will typically perform a physical examination (sometimes called a pelvic exam) and view your vaginal secretions under a microscope to identify any possible yeast or bacterial overgrowth.
If they do determine you have a yeast infection, they will likely suggest an antifungal medication. Many are available over the counter, but if your yeast infection is severe, they may prescribe a stronger antifungal. These medicines are available as topical creams, suppositories, or oral tablets.
Preventing Yeast Infections

Getting rid of a yeast infection is one thing. But as many women (and maybe possibly you!) know, keeping them from coming back is quite another.
Preventing yeast infections is not just about avoiding annoying or uncomfortable symptoms; it’s about maintaining your overall vaginal health. And the best ways you can maintain a balanced vaginal environment that supports overall vaginal health is through lifestyle practices like:
- Avoiding douching
- Practicing safe sex
- Wiping from front to back
- Wearing breathable cotton underwear
- Avoiding tight-fitting clothing, especially pants1
With yeast infection in particular, it’s also important to avoid a diet high in sugar, since sugar can fuel the growth (and overgrowth!) of yeast.
Incorporating Probiotics for Vaginal Health
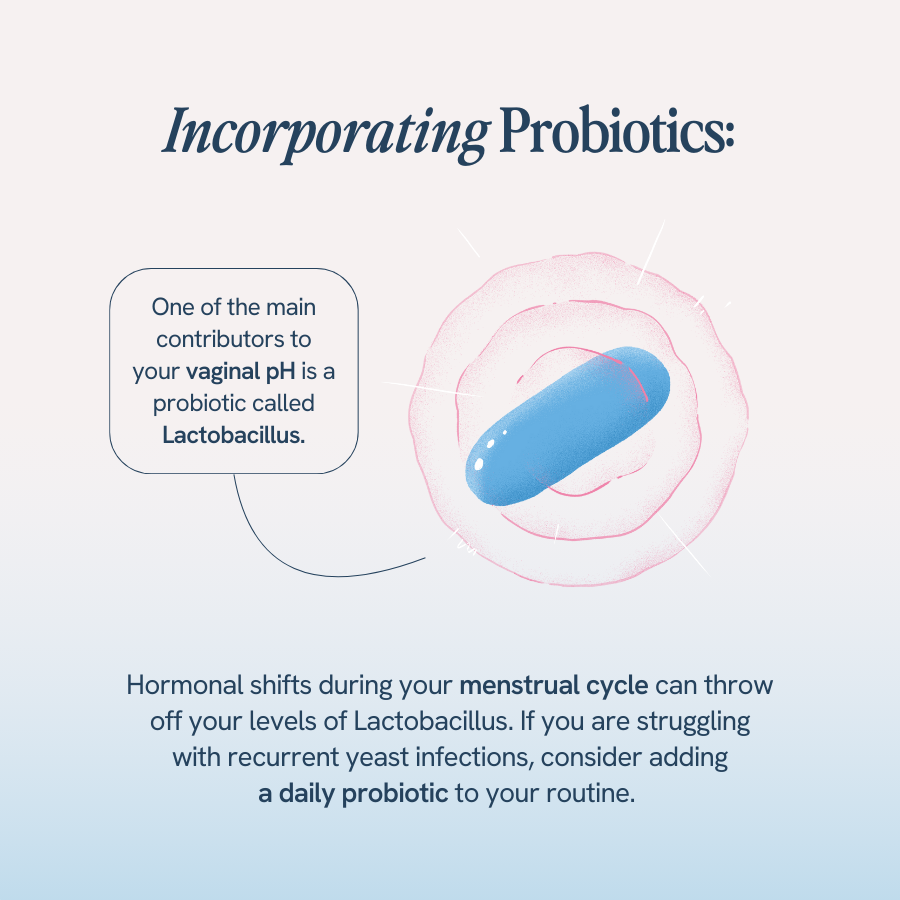
Remember how we said vaginal pH was important for fighting off bad, infection-causing microbes? Well, one of the main contributors to your vaginal pH is a probiotic called Lactobacillus. Lactobacillus releases lactic acid, which makes your pH slightly acidic to kill bad bacteria. However, hormonal shifts during your menstrual cycle can throw off your levels of Lactobacillus. This is where daily probiotics can help, especially Happy V’s Prebiotic + Probiotic.
Happy V’s Prebiotic + Probiotic is doctor-formulated to include clinically proven strains of Lactobacillus as clinically proven doses. By taking these clinically proven strains every day, you are ensuring you maintain a healthy, balanced vaginal microbiome throughout your menstrual cycle, one that can prevent the growth of harmful pathogens like yeast2.
Especially if you are struggling with recurrent yeast infections, consider adding a daily probiotic to your routine.
When to Seek Medical Help
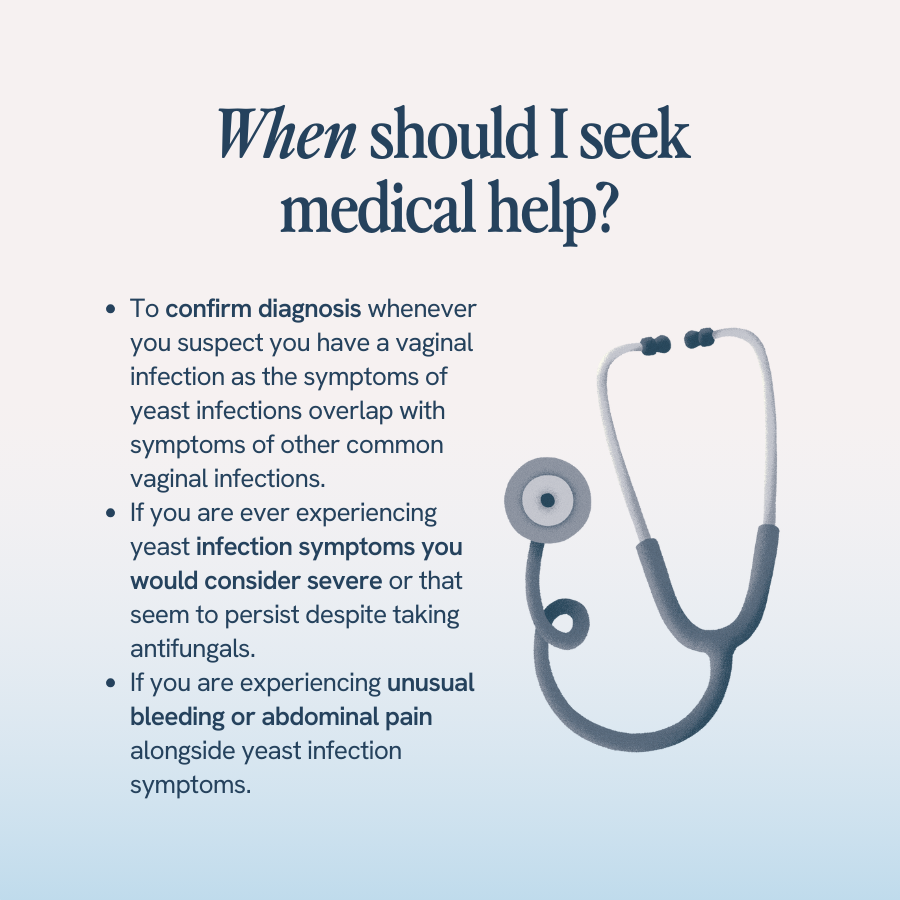
Whenever you suspect you have a vaginal infection, you should make an appointment with your doctor to confirm your diagnosis. The symptoms of yeast infections overlap with symptoms of other common vaginal infections, like BV or UTIs, but all require different forms of treatment to resolve.
Also, if you are ever experiencing yeast infection symptoms you would consider severe or that seem to persist despite taking antifungals, call your doctor. Lastly, never ignore unusual bleeding or abdominal pain alongside yeast infection symptoms. These are always signs to seek immediate medical attention.
- Yeast Infection: A vaginal infection caused by an overgrowth of fungus, particularly Candida albicans, leading to symptoms like itching, burning, redness, and abnormal discharge.
- Vaginal Microbiome: The community of microorganisms that naturally inhabit the vagina, which can be disrupted by yeast overgrowth.
- Menstrual Cycle: The monthly hormonal cycle in females, involving ovulation, thickening of the uterine lining, and shedding of the lining if pregnancy does not occur.
- Inflammation: A response of the body’s immune system to infection or irritation, characterized by redness, swelling, and pain.
- Vaginal pH: The level of acidity in the vagina, which plays a crucial role in preventing infections.
- Probiotics: Beneficial bacteria that help maintain a healthy balance of microorganisms in the body, including the vaginal microbiome.
- Lactobacillus: A type of probiotic bacteria that produces lactic acid, helping to maintain the acidic pH of the vagina and prevent overgrowth of harmful bacteria and yeast.
- Antifungal Medication: Treatment used to combat fungal infections like yeast infections, available in various forms such as creams, suppositories, or oral tablets.
- Recurrent Yeast Infections: Multiple episodes of yeast infections within a year, often requiring lifestyle changes and preventive measures for management.
- Vaginal Health: The overall well-being and maintenance of a healthy vaginal environment, crucial for preventing infections and promoting reproductive health.
- Yeast infection (vaginal). Mayo Clinic. January 11, 2023. Accessed May 2, 2024. https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999
- Menstrual Hygiene. Centers for Disease Control and Prevention. https://www.cdc.gov/hygiene/personal-hygiene/menstrual.html – Accessed November 24, 2023
- Mashatan N, Heidari R, Altafi M, Amini A, Ommati MM, Hashemzaei M. Probiotics in vaginal health [published correction appears in Pathog Dis. 2023 Jan 17;81:]. Pathog Dis. 2023;81:ftad012. doi:10.1093/femspd/ftad012. https://pubmed.ncbi.nlm.nih.gov/37286796/
- A-
- A+