- Antibiotics can be used to treat BV but they might also increase the chances of its recurrence.
- Antibiotics might cause dysbiosis in vaginal microflora, kill good bacteria, and eventually might lead to bacterial resistance.
- Metronidazole, Clindamycin, and Tinidazole are the first line of treatment options for BV.
- Some alternatives for BV prevention; Boric acid, Probiotics+Prebiotics, avoiding douching, avoid unprotected sex.
Let’s get one thing straight right off the bat: we aren’t anti-antibiotics. In fact, life could look pretty bleak without them, given that scientists estimate that there are more bacteria on Earth than stars in our entire galaxy. Antibiotics are an essential line of defense, especially against potentially life-threatening infections. But what about antibiotics for non-life-threatening infections like Bacterial Vaginosis?
In these cases, antibiotics are often referred to as those in the pharmaceutical world as “weapons of mass destruction.” This might sound dramatic, but it’s not totally off. Antibiotics work not by targeting and killing the bad bacteria in your body but by going in and killing all the bacteria in your body, both good and bad. When it comes to major infections, this is a necessary step. But in the instances of recurrent, non-life-threatening infections like BV, the overuse of antibiotics can increase the risk of bacterial resistance and cause adverse reactions.
If you are experiencing recurrent BV and feel like you’re stuck in the infection-antibiotic cycle, you’ve come to the right place. We’ll talk about effective, non-antibiotic treatments to end the frustration of BV once and for all.
What is Bacterial Vaginosis (BV)?
First, let’s talk about what bacterial vaginosis is and how it operates in your body. This will give you a better understanding for later.
Bacterial Vaginosis, also known as vaginitis or BV, is one of the top vaginal infections, affecting nearly 21 million women annually in the US. Though it can be transmitted through sexual activity and between sex partners, it’s not an STD or an STI. Bacterial vaginosis is actually caused by an overgrowth of bad bacteria like Gardnerella (2), and it’s this bacteria that can be passed from person to person.
The process of bad bacteria entering the vagina, overtaking the good bacteria, and causing possible infection is what The American College of Obstetricians and Gynecologists calls vaginal dysbiosis. Oftentimes, dysbiosis is preceded by a loss of beneficial bacteria through practices like unprotected sex or douching that can disrupt the vaginal flora.
Half of people with BV don’t experience any symptoms, but for those who do, symptoms include:
- Thin, milky white to grayish vaginal discharge
- Vaginal itching
- Foul vaginal odor, often described as a fishy smell(1)
If you want to know more about BV, check out our ultimate guide.
How do you treat BV?
As we said earlier, there’s only a 50% chance you experience any symptoms of BV, but even asymptomatic BV should be treated since BV has been linked to other health complications like preterm delivery and low birth weight during pregnancy, increased susceptibility to sexually transmitted infections, increased likelihood of infection after procedures like hysterectomy, and pelvic inflammatory disease (PID). (3) That’s why it’s so important to maintain regular appointments with your OB/GYN so they can screen for asymptomatic infections.
And if you do experience any of the symptoms of BV we mentioned above, that’s your sign to call your healthcare provider right away so they can get you started on a treatment plan.
There are two critical aspects of treating a BV infection:
- Killing the harmful bacteria and doing what you can to minimize the death of the good ones while doing so;
- And replenishing your stores of good bacteria, especially Lactobacillus and Bifidobacterium, which are the 2 bacteria most responsible for maintaining vaginal pH and women’s health
To achieve that first goal, most doctors prescribe a round of antibiotics.
What are common antibiotics for BV?
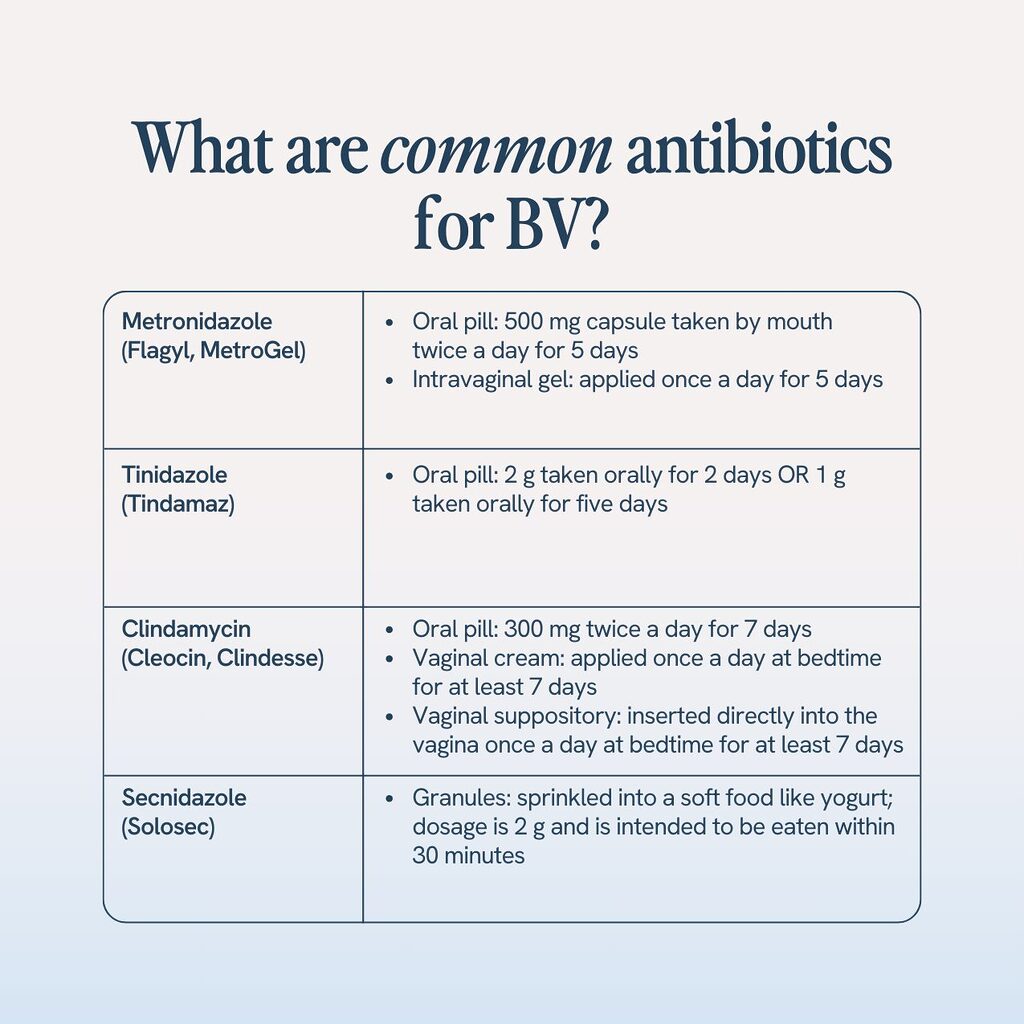
There are 2 antibiotics most commonly associated with BV: metronidazole and tinidazole. Metronidazole is often given as the first line of defense, and if the infection doesn’t clear after a full course, your doctor will likely prescribe tinidazole. We’ll talk about each a bit more in detail now, as well as some less common antibiotic treatments, but remember that if you have any questions about a medication your doctor is prescribing, you can always ask for more information. There’s no such thing as a stupid question, especially regarding your health.
1. Metronidazole (Flagyl, MetroGel)
Metronidazole, also known as Flagyl or Metrogel-Vaginal, is an antibiotic available as an oral pill and an intravaginal gel and is widely considered one of the best BV treatments. It became the drug of choice for BV thanks to its effectiveness in eradicating anaerobic vaginal bacteria. (4)
According to the Centers for Disease Control and Prevention (CDC), the general treatment plan for metronidazole involves either:
- A 500 mg capsule taken by mouth twice a day for 5 days
- A gel applied once a day for 5 days (5)
Possible side effects include nausea, vomiting, irritated GIT, appetite loss, metallic taste in the mouth, or headache.
2. Tinidazole (Tindamaz)
Tinidazole, also called Tindamax, is an oral BV treatment most likely prescribed if metronidazole does not clear the infection or causes a reaction.
CDC suggests two treatment strategies with tinidazole either:
- 2g taken orally for 2 days
- 1g taken orally for five days. (5)
Possible side effects include nausea, vomiting, abdominal cramping, a metallic taste in the mouth, loss of appetite, dizziness, headache, and constipation. It’s also recommended that you avoid any alcohol while on tinidazole and for at least 3 days after the course has been completed.
3. Clindamycin (Cleocin, Clindesse)
Clindamycin, also called Cleocin or Clindesse, comes as a pill, a vaginal cream, and a vaginal suppository inserted directly into the vagina.
The CDC’s treatment guidelines vary based on if you are using a pill, cream, or suppository:
- If applied intravaginally as a cream or ovule suppository, apply once a day at bedtime for at least 7 days
- If taken orally, take 300 mg twice a day for 7 days (5)
Possible side effects include nausea, vomiting, pain in the joints, pain while swallowing, heartburn, metallic taste in the mouth, and itching of the vagina. You should also avoid using latex condoms if using a cream or suppository, as it can be more likely to tear.
4. Secnidazole
Secnidazole, also called Solosec, is a BV treatment in granules. It’s a new, single-dose treatment approved by the FDA in 2017. It is more expensive than other options, but many find it worth the cost to only have to remember to take one dose.
As a granule, secnidazole is meant to be sprinkled into a soft food like yogurt. The dosage is typically 2g and is intended to be eaten within 30 minutes.
Possible side effects include nausea, vomiting, diarrhea, a metallic taste in the mouth, and headache.
What do antibiotics do to your body and your vagina’s ecosystem?
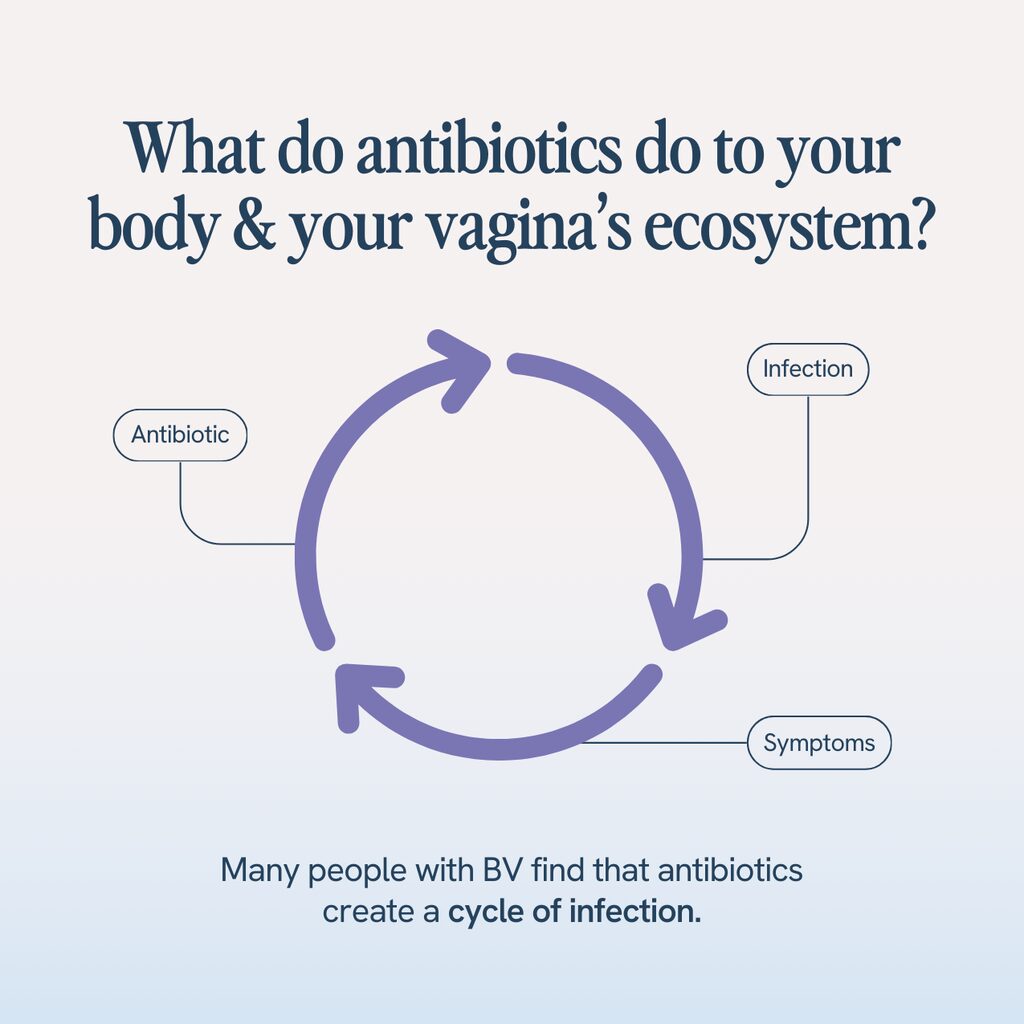
The antibiotics used to treat BV are called “broad spectrum” antibiotics, which means they kill a broad spectrum of bacteria, both good and bad.
Many people with BV find that antibiotics create a cycle of infection. Without good bacteria left in your vaginal flora to fight off the bad, you are actually more susceptible to developing recurrent bacterial vaginosis or another common vaginal infection, like a vaginal yeast infection.
If you’ve been struggling with recurring BV and feeling like you are doing something wrong, chances are, you aren’t. It may be a sign that it’s time to discuss more natural treatment options with your healthcare provider.
How can you get rid of BV without antibiotics?
The good news is that there are proven ways of eradicating BV that don’t involve antibiotics. It’s always a good idea to talk to your healthcare provider before beginning any alternative treatments, so they can discuss and help monitor treatment.
1. Prebiotics + Probiotics
Probiotics are one of the more effective natural treatment and prevention strategies when it comes to BV because probiotics actively help replenish your body’s stores of healthy bacteria, particularly a probiotic known as Lactobacillus, which is the bacteria most responsible for killing harmful microbes and maintaining overall vaginal wellness.
Probiotics naturally occur in foods like yogurt, kefir, and kimchi, but those struggling with BV find it easier to take a daily probiotic supplement.
Supplements containing Lactobacillus are a must for reasons we’ve already mentioned. But, many find their probiotics to work more effectively when combined with a prebiotic. Which makes sense. Prebiotics are essentially fibers that aren’t digested by your body and begin to ferment. The fermentation supplies food for the beneficial bacteria or probiotics to thrive.
If a supplement sounds like something you want to try, save yourself some research and try Happy V’s Prebiotic + Probiotic. It meets all the qualifications we just mentioned, plus we’ll ship it straight to your door.
2. Boric Acid Suppositories
Boric acid is the most commonly used over-the-counter BV medication. It’s inexpensive and can be purchased at practically any pharmacy.
One study showed that boric acid effectively treated active BV infections, with 88-92% of the women being cured of BV within 7 to 12 weeks of treatment. (8) Boric acid, however, does not help replenish your vaginal flora in the same way that probiotics do.
Boric acid does have a long treatment timeline, too. According to the guidelines of the CDC, boric acid can be applied for 21 days at a dose of 600mg per day to avoid the recurrence of BV. (5)
3. Change eating & drinking habits

If you are struggling with recurrent BV, it may be time to examine your diet. Is it high in the three S’s (salt, sugar, and saturated fat)? How many alcoholic drinks are you consuming per week?
Studies show that limiting these S-foods and reducing alcohol intake can decrease the recurrence of BV, as all these things provide foods that bad bacteria love to eat.
4. Avoid douches, vaginal soaps and cleansers
Believe it or not, the vagina is self-cleaning, making most of these products flat-out unnecessary.
But more than that, when you introduce chemicals into the vaginal through douching or scented cleaners, you are potentially altering your vaginal flora, which makes you more prone to imbalances that lead to infection.
If you ever want to clean that area, simply opt for warm water and mild, unscented soap. And if you ever do experience an unusual odor or fishy smell, don’t try to cover it up with a vaginal deodorant. Call your doctor to find the root cause.
5. Practice good sex hygiene
Everyone has a different microbiome, filled with good bacteria as well as bad. And when we have sex with someone, especially unprotected sex, we expose our microbiome to theirs, which can be a potential infection risk.
So avoid multiple sexual partners and use protection like latex-free condoms, since latex condoms can irritate your vaginal mucosa.
Along with that, it’s a good idea to:
- Rinse your genital area with water after having intercourse.
- Pee right after having sex.
- Use paraben-free lube to avoid irritating chemicals common in most lubes
- Express concerns about your health with your partner so you can come up with a solution together
6. Wear breathable cotton underwear
Harmful bacteria love dark, damp environments. And underwear made of synthetic materials like silk or nylon create these environments by not allowing your vagina to breathe. Swap synthetic undies for natural cotton.
According to WebMD the American College of Obstetricians and Gynecologists, wearing cotton undies lowers your risk of getting BV because it is light and breathable for your skin.
7. Avoid fads
But wait… what about apple cider vinegar? Hydrogen peroxide? Tea tree oil?
At Happy V, we put science first. And though these remedies are all gaining traction, the evidence just isn’t there to support them. If you are going to pursue a natural treatment for BV, stick to the things we’ve listed above.
Can bacterial vaginosis clear up on its own?
Sometimes, yes. In 1 out of every 3 instances of BV, it clears up on its own with no need for any antibiotics or other forms of treatment.
However, if you are experiencing any symptoms of BV, like itching, discharge, or fishy odor, that’s a sign your body needs additional help to fight the infection. And it’s better to seek treatment sooner than later since an active BV infection makes you more prone to sexually transmitted diseases and can lead to complications for pregnant women. And remember, your health is in your hands. If your doctor prescribes antibiotics and that makes you uncomfortable, you can talk with them about the home remedies we mentioned here and see if any are viable alternatives. And if an antibiotic prescription is unavoidable, consider offsetting the effects with a high-quality daily probiotic supplement. With a probiotic supplement like Happy V’s Prebiotic + Probiotic, you can finally break the cycle of antibiotics and recurring BV and enjoy better vaginal health.
Our Happy V® Prebiotic + Probiotic was created for anyone who is experiencing symptoms related to Bacterial Vaginosis and Yeast Infections. Eliminate the odor, itch, gut bloating, and other symptoms.
Bacterial resistance – Ability of bacteria to resist the action of medication intended to kill or stop it.
Dysbiosis – Imbalance in microbial flora
Facultative bacteria – Bacteria that can grow with or without oxygen
Anaerobic bacteria – Bacteria that can grow in the absence of oxygen and are capable of causing disease.
- Van den Munckhof, E. H., van Sitter, R. L., Boers, K. E., Lamont, R. F., te Witt, R., le Cessie, S., … & Leverstein-van Hall, M. A. (2019). Comparison of Amsel criteria, Nugent score, culture and two CE-IVD marked quantitative real-time PCRs with microbiota analysis for the diagnosis of bacterial vaginosis. European Journal of Clinical Microbiology & Infectious Diseases, 38(5), 959-966.
- Mårdh P. A. (1993). Définition et épidémiologie des vaginoses bactériennes [The definition and epidemiology of bacterial vaginosis]. Revue francaise de gynecologie et d’obstetrique, 88(3 Pt 2), 195–197.
- Centers for Disease Control and Prevention. Bacterial vaginosis statistics. https://www.cdc.gov/std/bv/stats.htm
- Sonja Löfmark, Charlotta Edlund, Carl Erik Nord, Metronidazole Is Still the Drug of Choice for Treatment of Anaerobic Infections, Clinical Infectious Diseases, Volume 50, Issue Supplement_1, February 2010, Pages S16–S23, https://doi.org/10.1086/647939
- Centers for Disease Control and Prevention. Bacterial vaginosis treatment guidelines. https://www.cdc.gov/std/tg2015/bv.htm
- NIH. U.S. National Library of Medicines. Medline Plus (Clindamycin). https://medlineplus.gov/druginfo/meds/a682399.html
- Mayer, B. T., Srinivasan, S., Fiedler, T. L., Marrazzo, J. M., Fredricks, D. N., & Schiffer, J. T. (2015). Rapid and Profound Shifts in the Vaginal Microbiota Following Antibiotic Treatment for Bacterial Vaginosis. The Journal of infectious diseases, 212(5), 793–802. https://doi.org/10.1093/infdis/jiv079
- Reichman, O., Akins, R., & Sobel, J. D. (2009). Boric acid addition to suppressive antimicrobial therapy for recurrent bacterial vaginosis. Sexually transmitted diseases, 36(11), 732–734. https://doi.org/10.1097/OLQ.0b013e3181b08456
- Markowiak, P., & Śliżewska, K. (2017). Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients, 9(9), 1021. https://doi.org/10.3390/nu9091021
- Bilardi, J., Walker, S., McNair, R., Mooney-Somers, J., Temple-Smith, M., Bellhouse, C., Fairley, C., Chen, M., & Bradshaw, C. (2016). Women’s Management of Recurrent Bacterial Vaginosis and Experiences of Clinical Care: A Qualitative Study. PloS one, 11(3), e0151794. https://doi.org/10.1371/journal.pone.0151794
- A-
- A+






